
IDAHO MEDICAID
HEALTH PLAN BOOKLET
2020
Table of Contents
WELCOME TO THE IDAHO MEDICAID HEALTH PLAN ......................................... 1
WELCOME ..................................................................................................................................... 1
DISCLAIMERS ................................................................................................................................ 1
PRIVACY NOTES ............................................................................................................................ 2
INFORMATION TO REMEMBER ....................................................................................................... 2
WHAT ARE MY RESPONSIBILITIES? .................................................................... 3
HOW DO I APPLY FOR MEDICAID? ...................................................................... 3
GETTING AN APPLICATION ............................................................................................................ 3
COMPLETING YOUR APPLICATION ................................................................................................. 4
TURNING IN YOUR APPLICATION ................................................................................................... 4
HOW TO GET IDAHO MEDICAID FOR WORKERS WITH DISABILITIES ............................................... 5
HOW DO I ACCESS WOMEN'S HEALTH CHECK FOR BREAST AND CERVICAL CANCER SCREENING? .. 5
WHAT DO I NEED TO KNOW ABOUT MY IDAHO MEDICAID IDENTIFICATION
CARD? ................................................................................................................... 6
WHAT DO I NEED TO KNOW ABOUT IDAHO MEDICAID BENEFIT PLANS? ......... 7
MEDICAID VS. MEDICARE ............................................................................................................. 8
IDAHO MEDICAID HEALTH PLAN - THE BASIC PLAN ...................................................................... 9
IDAHO MEDICAID HEALTH PLAN - THE ENHANCED PLAN............................................................. 17
IDAHO MEDICAID HEALTH PLAN - THE MEDICARE-MEDICAID COORDINATED PLAN .................... 19
HEALTHY CONNECTIONS PRIMARY CARE PROGRAM .................................................................... 20
REFERRALS................................................................................................................................. 22
EMERGENCY CARE ...................................................................................................................... 25
CRISIS SERVICES ......................................................................................................................... 25
POISON CONTROL ....................................................................................................................... 26
URGENT CARE ............................................................................................................................ 26
EARLY AND PERIODIC SCREENING, DIAGNOSTIC, AND TREATMENT (EPSDT) .............................. 26
PRIOR AUTHORIZATION .............................................................................................................. 27
WHAT DO I NEED TO KNOW ABOUT PAYING FOR SERVICES? ......................... 28
COPAYMENTS .............................................................................................................................. 28
NO SHOW OR MISSED APPOINTMENTS ........................................................................................ 29
PREMIUMS.................................................................................................................................. 29
NON-COVERED SERVICES ........................................................................................................... 29
WHAT OTHER INFORMATION DO I NEED TO KNOW? ...................................... 30
OTHER MEDICAL INSURANCE ..................................................................................................... 30
HEALTH INSURANCE PREMIUM PAYMENT PROGRAM ................................................................... 30
YOUR RIGHTS .............................................................................................................................. 31
FRAUD, ABUSE, AND MISUSE ...................................................................................................... 34
ESTATE RECOVERY ..................................................................................................................... 34
WHO CAN I CALL IF I HAVE QUESTIONS OR NEED INFORMATION? ................ 36
LOCAL HEALTHY CONNECTIONS OFFICES .................................................................................... 38
REGIONAL PROGRAM OFFICES .................................................................................................... 40
1
Welcome to the Idaho Medicaid Health Plan
Welcome
Welcome to Idaho Medicaid.
You are receiving this booklet because you are eligible for Idaho Medicaid and we want
you to get the healthcare that meets your needs.
Idaho Medicaid is administered by the Idaho Department of Health and Welfare’s
Division of Medicaid. This booklet will answer many of the questions you may have
about getting started with Idaho Medicaid and using your benefits. People are different,
and so are their healthcare needs.
Idaho offers three different benefit plans based on your healthcare needs. This booklet
tells you about your coverage under the Basic, Enhanced, or Medicare-Medicaid
Coordinated healthcare plans through June 30, 2021. It explains healthcare services,
behavioral health (mental health and substance use disorder) services, prescription drug
coverage, and long-term services and supports. It also includes phone numbers for our
programs, so you know who to call when you have questions.
No matter which plan you are enrolled in, it is important to use your healthcare services
wisely. We want to help you improve your health, find health issues early, and manage
your current health issues. You can help by making healthy choices that help you stay
well and make your health plan work for you.
Disclaimers
When this booklet says “we,” “us,” or “our,” it means the Idaho Department of Health
and Welfare and its divisions (like the Division of Medicaid). This booklet will introduce
you to coverage information and explain your rights and responsibilities. Please be
advised this booklet does not create any legal rights or entitlements. You should not rely
on this booklet as your only source of information about Idaho Medicaid. You can get
more detailed information about Idaho Medicaid and rules by looking at the Idaho
Department of Health and Welfare website and Idaho Medicaid’s website.
2
Privacy Notes
Never give personal information, like your Social Security number or banking
information, to someone who calls or emails you asking for it. We will not contact you
directly for information about your Idaho Medicaid identification card to verify your
identity.
Idaho Medicaid uses, and shares protected health information with your healthcare
providers to provide health benefits, to treat, pay, and provide healthcare services, and
for other reasons allowed and required by federal and state laws. However, we keep your
health information private and limit access as required by federal and state laws.
To read Idaho’s privacy policy, go to https://www.idaho.gov/about-us/privacy-policy/.
Information to Remember
We are here to help and available from 8 a.m. to 5 p.m. Monday through Friday. You can
also visit us online at https://healthandwelfare.idaho.gov/default.aspx any time. See
pages 36-40 for contact information, a list of services, programs, units, contractors, and
organizations listed throughout this health plan booklet.

3
What Are My Responsibilities?
When you apply for benefits you agree to give true,
correct, accurate, and up-to-date information.
Below is a list of some of your responsibilities as an
Idaho Medicaid Health Plan participant.
As an Idaho Medicaid participant you agree to
report any of the following changes as soon as
possible:
• You have a new name, address, or other contact information.
• Someone moves in or out of your household (even if they aren’t related to you).
• You marry, divorce, become pregnant, or have a child (including adoptions).
• Your income goes up or down (including child support, unemployment, job wages,
etc.).
• You get or lose other health insurance (including Medicare coverage).
Read all letters and notices that you receive. Letters have important information for you
about your eligibility, services, and benefits. If you have problems reading or
understanding the letters or information, call and ask for help.
Call Idaho Department of Health and Welfare’s toll-free Benefits Customer Service
center line at 877-456-1233 to report any changes.
How Do I Apply for Medicaid?
Getting an Application
To apply for Medicaid, please complete an application.
You can do this by:
• Calling the Idaho Department of Health and Welfare’s toll-free Benefits Customer
Service center line at 877-456-1233 to apply over the phone.
• Going to your local Health and Welfare office
https://healthandwelfare.idaho.gov/ContactUs/tabid/127/Default.aspx.
• Visiting https://idalink.idaho.gov/, https://www.yourhealthidaho.org/, or
https://www.livebetteridaho.org/.
• Calling the Idaho CareLine at 2-1-1 or 800-926-2588 and requesting an application.
4
Completing Your Application
As you fill out your application, it is important for you to know that:
• You can get an application in English or Spanish.
• Language interpretation is available at 877-456-1233.
• TTY/TDD is available by calling 888-791-3004.
• Parents and guardians can apply for their children.
• Friends and relatives can help you fill out the application.
Turning in Your Application
After your application is complete, there are several ways to return it, online, over the
phone, in-person or by mail, email or fax:
• Online by visiting https://idalink.idaho.gov/, https://www.yourhealthidaho.org/, or
https://www.livebetteridaho.org/.
• Over the phone at 877-456-1233.
• Email your application to [email protected].
• In-person at any local Health and Welfare office
https://healthandwelfare.idaho.gov/ContactUs/tabid/127/Default.aspx.
• Fax your application to 866-434-8278.
• Mail your application to: Department of Health and Welfare, Self-Reliance
Programs, PO Box 83720, Boise, ID 83720-0026.
After you turn in your application, your case will be reviewed by our staff to see if you
are eligible for Medicaid. If we need more information, we will call you or send you a
letter asking for it. It is important for you to tell us if your phone number, address, or
email change. If you completed your application over the phone or online, you don’t
have to submit a paper application.
Once your application is received, it usually takes us about 45 days to determine
eligibility. If we need more information, this may extend the time frame. We will let you
know if we need more information.
Once we have determined eligibility, you will get a letter notifying you if you are eligible
for Medicaid. If you are eligible and are new to Medicaid, you will be mailed a Medicaid
identification card within 2 weeks. Your identification card is permanent. Do not throw
it away, ever. If you lose benefits and then get benefits again, you will use the same card.
If you have questions about your application or need to give us your new address or
phone number, you can call 877-456-1233.
5
How to get Idaho Medicaid for Workers with Disabilities
Idaho Medicaid has a health insurance program for people who work and have a
disability. When you apply, please write Medicaid for Workers with Disabilities
on the top of your application.
You might qualify for Medicaid for Workers with Disabilities if you:
• Have a disability (defined by the Social Security Administration).
• Are between 16 and 64 years old.
• Have a job or are self-employed.
• Are a resident of Idaho.
• Meet income requirements and resource limits restrictions.
If you have questions or would like more information, visit
https://healthandwelfare.idaho.gov/Medical/Medicaid/MedicaidforWorkerswithDisabi
lities/tabid/1917/Default.aspx. See page 3 for how to apply or call Idaho Department of
Health and Welfare’s toll-free Benefits Customer Service center line at 877-456-1233.
How Do I Access Women’s Health Check for Breast and Cervical Cancer
Screening?
Some women might qualify for free breast and cervical health screening. You might
qualify if you are:
• Low income.
• Do not have insurance coverage for mammograms or Pap tests.
• Age 50 to 64.
• Age 21 to 49 and are due for a cervical cancer screening or are referred by a doctor
for symptoms suspicious for breast cancer.
Call the Idaho CareLine at 2-1-1 or 800-926-2588 to connect with a Women’s
Health Check provider to see if you qualify.
6
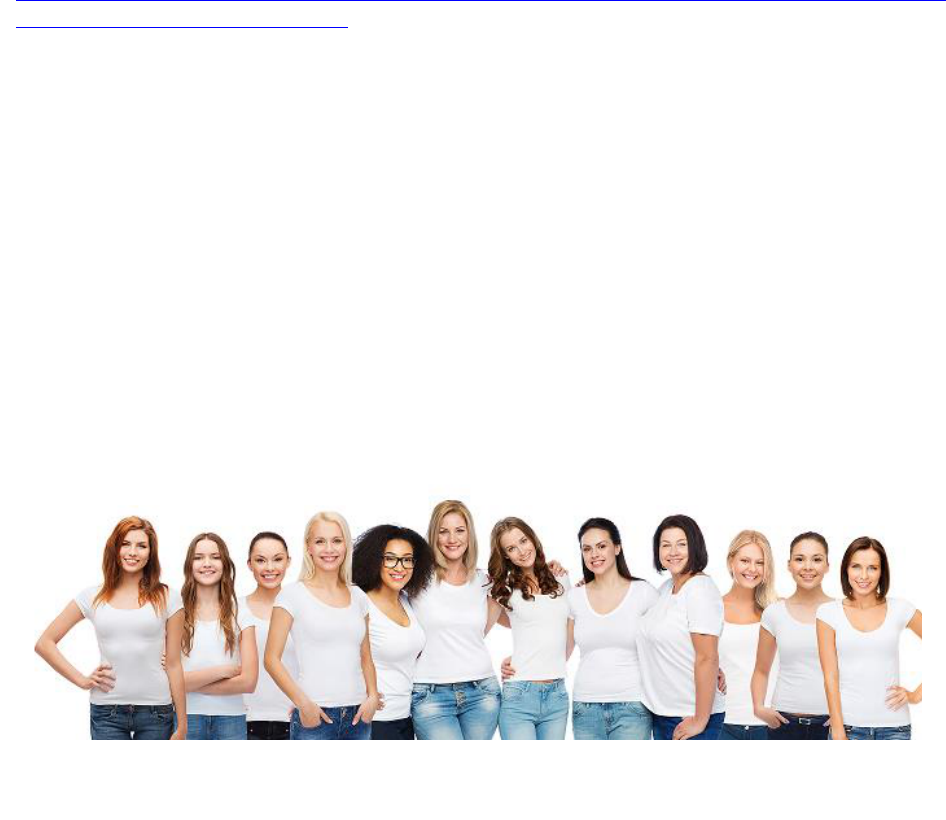
What Do I Need to Know About My Idaho Medicaid Identification
Card?
The first time you are eligible for Idaho Medicaid, you will receive an identification card
in the mail. If you are eligible and have not received your card within 14 days of
receiving your letter, please call 877-456-1233.
It is important to remember:
• Keep your card in your purse or wallet so you will have it with you to show to your
doctor, dentist, or pharmacy. You might have to show picture identification in
addition to your Medicaid card.
• Always show your identification card and ask before you get medical services if the
provider will accept your identification card as payment. Ask even when your doctor
refers you to a specialist. Not all doctors accept Idaho Medicaid.
• Report name changes to your local Health and Welfare office by calling
877-456-1233. Your card may not work at providers’ offices if you are going by a
different name than what appears on your identification card.
• Your identification card is permanent. Do not throw it away, ever. If you lose benefits
and then get benefits again, you will use the same card.
• If you lose your card, call the Department of Health and Welfare at 877-456-1233 or
call the DXC participant line at 866-686-4752.
7
What Do I Need to Know About Idaho Medicaid Benefit Plans?
Idaho Medicaid administers comprehensive healthcare coverage for eligible Idahoans.
Medicaid contracts with individual healthcare providers, agencies, institutions, and
managed care entities to provide healthcare services for low-income people and
families, including children, pregnant women, the elderly, and people with disabilities.
Medicaid participants have access to covered benefits through three plans that align
with health needs:
• The Basic Plan is designed to meet the health needs of people in generally good
health, without disabilities or special health needs. This plan provides health,
prevention, and wellness benefits. Most participants will be in this benefit plan.
• The Enhanced Plan is for people with more complex needs and medical
conditions, disabilities or special health needs, and people over the age of 65. This
plan has all the benefits of the Basic Plan, plus developmental disability services,
children’s service coordination, and long-term services and supports.
• The Medicare-Medicaid Coordinated Plan is for people who are eligible and
enrolled in both Medicare and Medicaid, also known as dual eligibles. This plan has
all the benefits of the Enhanced Plan, plus allows people to enroll in a managed care
plan to help coordinate Medicare and Medicaid benefits. There are many advantages
to enrolling in managed care, one of the most valuable is access to a care coordinator
who assists people with complex medical conditions to achieve better health.
Health and Welfare has partnered with insurance companies to administer and
provide coordinated health coverage between Medicare Part A (hospital insurance),
Part B (medical insurance), Part D (drug coverage), and Medicaid through Medicare
Advantage plans. There is no cost to you when you follow the plan rules and
requirements.
For more information you can visit Medicare at the links below:
- Part A https://www.medicare.gov/what-medicare-covers/what-part-a-covers
- Part B https://www.medicare.gov/what-medicare-covers/what-part-b-covers
- Part D https://www.medicare.gov/drug-coverage-part-d
- Medicare Advantage Plans https://www.medicare.gov/sign-up-change-
plans/types-of-medicare-health-plans/medicare-advantage-plans

8
Medicaid vs. Medicare
People sometimes confuse Medicaid and Medicare. They are
not the same, but they do work together to provide benefits
for some Idaho residents who qualify for both.
Medicaid
Medicaid is a state program you might qualify for if:
• You are any age and your income makes you eligible to receive Medicaid benefits.
• You are a child under age 19.
• You are an adult with an eligible child.
• You are blind or disabled (based on Social Security criteria).
• You are age 65 or older.
If you or someone in your family needs healthcare, you should apply for Medicaid even
if you are not sure you qualify. Some income and resources are not counted when
determining your eligibility. For example, owning your home might not prevent you
from getting Medicaid.
Medicare
Medicare is a federal program you might qualify for if:
• You are age 65 or older.
• You are age 18 or older with ESRD (End-Stage Renal Disease, permanent kidney
failure requiring dialysis or transplant).
• You have ALS (Amyotrophic Lateral Sclerosis, also called Lou Gehrig’s disease).
• You are a younger person with a permanent disability.
Some people qualify for both Medicaid and Medicare. If you are eligible for both, you
may also be able to enroll in the Medicare-Medicaid Coordinated Plan. See page 19 for
more information.
Some people who do not qualify for full Medicaid benefits are eligible for Qualified
Medicare Beneficiary programs https://www.benefits.gov/benefit/6177, where
Medicaid helps pay for Medicare costs including:
• Monthly Medicare premiums.
• Co-insurance.
• Deductibles.
For more information, visit the Medicare website at https://www.medicare.gov/ or call
800-633-4227.
9
Idaho Medicaid Health Plan - The Basic Plan
The Basic Plan is for people with generally good health, without disabilities or special
health needs. This plan provides health, prevention, and wellness benefits. Most
participants will be in this benefit plan.
Here is a summary of the services you may be eligible for if you are on the Basic Plan:
• Behavioral health
• Chiropractic
• Counseling
• Dental
• Doctors and other healthcare
providers
• Durable medical equipment and
supplies
• Early intervention
• Early and Periodic Screening,
Diagnostic, and Treatment (EPSDT)
• Hearing
• Home health
• Hospital
• Immunizations
• Interpretation
• Lead screening
• Nutrition
• Physical, occupational, and speech
therapy
• Podiatry
• Pregnancy and family planning
• Prescription drugs
• Preventive Health Assistance
• School-based
• Substance use disorder
• Transportation
• Vision
• Wellness exams for adults
• Wellness exams for children
Keep in mind that there are some limits to these services, and some might require you
or your healthcare provider to get prior authorization from Medicaid.
If you are enrolled in the Basic Plan and your health changes, you might need to get an
assessment to see if you qualify for the Enhanced Plan to receive additional services.

10
Brief Description of the services available through the Basic Plan:
Behavioral Health
If you have a behavioral health condition (like depression, anxiety, substance use,
or other mental health conditions), Medicaid through the Idaho Behavioral Health
Plan offers outpatient behavioral healthcare services that include:
• Community-based treatment and
rehabilitation services
• Assessment and planning
• Psychological and
neuropsychological testing
• Psychotherapy (individual, group,
and family)
• Medication management
• Partial care treatment
• Substance use disorder treatment
• Alcohol/drug screening
• Partial hospitalization
• Intensive outpatient program and
case management
Services are available when medically necessary to meet an individual’s treatment
needs and are provided by professionals enrolled in the Optum Idaho provider
network.
Call Optum Idaho at 855-202-0973 or visit the Optum Idaho website at
https://www.optumidaho.com/ for more details.
Chiropractic
• Limited to 6 visits during a calendar year.
- Does not pay for x-rays taken by a chiropractor.
Counseling
• See Behavioral Health.
Dental
These benefits are covered by Medicaid through a dental insurance program called
Idaho Smiles. MCNA Dental is the managed care contractor that administers and
manages Medicaid dental benefits, including emergency dental conditions, and
pain management.
• Idaho Smiles covers the following dental care:
- Children and young adults up to age 21 years for basic and preventive dental
care, which includes exams, x-rays, fillings, oral surgery, orthodontics when
necessary, emergency dental care, restorative services, and other medically
necessary treatment.
- Adults, age 21 years and over, for basic and preventive dental care, which
includes exams, x-rays, fillings, oral surgery, dentures, and other medically
necessary treatment. Root canals and crowns are not covered for adults.
11
For more information, call the MCNA Dental customer service line at 855-233-6262
or visit the MCNA website at https://www.mcnaid.net/en/home/.
Doctors and Other Healthcare Providers
• Office visits.
• Exams or treatments by a doctor, physician assistant, or nurse practitioner.
• Surgical and other treatments performed by a doctor.
• Diagnostic lab and radiology.
Durable Medical Equipment and Supplies
• Prescribed by a doctor.
• Artificial limbs and braces.
- To replace portions of the body
that are weak or missing.
• Special shoes or inserts for
diabetics.
• Wheelchairs.
• Oxygen and oxygen equipment.
Early Intervention
• Children from birth to age 3 years.
- Developmental screening and assessments.
- Physical, occupational, and speech therapy.
- Family training and counseling in the natural environment.
Early and Periodic Screening, Diagnostic, and Treatment (EPSDT)
• If you are under the age of 21 years and your doctor says you need medical
services not covered in your plan, Medicaid may prior authorize the medically
necessary services for you. See page 26 for more information about EPSDT.
Hearing
• Adults
- Hearing tests are covered when your doctor cannot determine the cause for
your hearing loss.
- Hearing aids for adults are not covered.
• Children and young adults up to age 21
- Replacement hearing aids with prior authorization.
- Exam and testing once each calendar year when ordered by a doctor.
- Batteries, follow-up testing, and repairs from normal use.
- Lost, misplaced, stolen, or destroyed hearing aids are not covered.
12
Home Health
• When ordered by a doctor
- Limited to 100 visits during a calendar year, including all visits such as skilled
nursing, aide visits, physical therapy, occupational therapy and speech
language pathology therapy.
Hospital
Your doctor might need to get prior authorization for some hospital services from
Medicaid’s Quality Improvement Organization. For more information, call
866-538-9510.
• Inpatient
- Semi-private room, prescription drugs, lab tests, and other medically
necessary services.
- Lab, x-ray, and other tests ordered by your doctor.
- Physical therapy and other services ordered by your doctor.
- Psychiatric services.
• Outpatient
- Diagnostic and treatment services.
- The emergency room is not for routine medical care. If you are not sure you
have an emergency, call your doctor for medical advice.
Immunizations
• Provided in your healthcare provider’s office, a doctor’s office, pharmacy, a free
clinic, or through your local public health district.
• Ask to have your child’s immunizations recorded into Idaho’s Immunization
Reminder Information System (IRIS). This system is a secure health information
system containing the names and immunization history of people who have
received vaccinations in Idaho. This information is available only to authorized
healthcare providers, child care providers, and schools.
Interpretation
• Your doctor, dentist, mental health, or other healthcare providers are responsible
for providing interpreters if you need help communicating about your health
services. You cannot be billed for those services.
Lead Screening
• Your doctor should test your child for lead at 12 months old and again at 24
months. Anyone under the age of 21 years should be tested if they have not been
tested.
• Your child can have lead poisoning and not seem sick. Lead poisoning can lower a
child’s intelligence and ability to learn.
13
Nutrition
• Nutritional services for pregnant women and children.
• Nutritional support therapy when medically necessary and ordered by a doctor.
• Diabetes education.
- Limited to 12 individual hours or 24 group hours every five years.
Physical, Occupational, and Speech Therapy
• Covered as an outpatient hospital service, in schools, and by independent
therapists.
• Some service limits apply. Your therapist may be able to continue treatment
beyond service limits under some circumstances.
• Inform your therapist any time you receive therapy services from another
provider to avoid problems with service limits.
Podiatry
• Care of your feet and ankles.
- Limited to severe conditions from your mid-calf down.
- Limited to routine foot care for chronic disease-related care (such as
diabetes).
Pregnancy and Family Planning
• Pap test performed during family planning or at yearly physical.
• Family planning, counseling, prescriptions, and supplies to prevent pregnancy.
• Sterilization (includes vasectomies and tubal ligations).
- You must sign legal consent forms at least 30 days in advance. You can have
the surgery on the 31st day.
- Does not pay for sterilization if the person is under the age of 21 years, or if
the person is not capable of giving informed consent.
• Prenatal, delivery, and postpartum services provided by a doctor, an RN certified
nurse midwife, or a licensed midwife.
• Fertility services or medications for the inducement of fertility are not covered.
Prescription Drugs
• Idaho Medicaid health plans cover medicines prescribed by your doctor unless
they are covered by Medicare.
- Some types of medicines and some brand name prescription drugs require
prior authorization. Your pharmacist or provider will know which medicines
need prior authorization and will submit the request for you.
• Some non-prescription items are covered if your doctor orders them.
14
Preventive Health Assistance (PHA)
• Weight Management PHA benefits.
- Weight Management PHA must be recommended to you by your doctor if you
have a body mass index either in the obese range or the underweight range.
- If you qualify for PHA, you can earn points and use them to pay for services to
help you achieve a healthy weight.
- Maximum benefit is 200 points a year (1 point = $1).
• Wellness PHA benefits (Children up to the age of 19 and enrolled in Children’s
Health Insurance Program).
- If you pay a monthly $10 or $15 premium for your child’s health plan you can
reduce your monthly bill by $10 per month by earning PHA points. PHA
points are awarded when you keep your child’s wellness exams and
immunizations up to date.
- Points can only be used to pay your monthly premium.
School-Based
• The school might test your child and determine that your child is eligible for
services under an Individualized Educational Plan (IEP) or Individualized Family
Services Plan.
• With your permission, your child’s school can bill Medicaid for the services.
• Services listed on your child’s plan are counted separately from services your
child might be getting in other places.
• Ask your child’s school if they bill Medicaid.
• Give your child’s identification number and the name of your child’s doctor to the
school.
• Tell the school if your child is working with other therapists or doctors.
Substance Use Disorder
• See Behavioral Health.
Transportation
Non-Emergency Medical Transportation (NEMT)
If you have a medical appointment but you do not have a car, cannot operate a car,
or do not have a friend or family member who can take you, you can request
transportation through Medicaid’s non-emergency medical transportation
provider, MTM.
• If you have a vehicle to transport yourself or family members to their
appointments, please contact MTM and ask about their mileage reimbursement
program.
• MTM will review your request and decide if Medicaid will pay for your
transportation. MTM will review your request based on the least expensive
transportation available and the closest available Medicaid provider for the
service.
15
• If you have been referred for medical care outside your community, MTM might
ask for a referral from your doctor before they will schedule your transportation.
• You need to call at least 48 hours before your appointment.
Call MTM toll free at 877-503-1261 or visit the MTM website at https://www.mtm-
inc.net/idaho/.
Vision
• For adults age 21 and older.
- Limited to treatment for acute needs such as removal of foreign objects in the
eye.
- Adults with chronic diseases such as diabetes or glaucoma that require regular
eye care can get eye exams once every year.
• For children and young adults under age 21 years.
- Covers frames and lenses when needed.
- The doctor who does the exam might not be the provider who supplies your
glasses. Be sure to ask if your doctor orders glasses from the Medicaid
supplier.
- Does not pay for transition or progressive lenses for any age, or tints unless an
extreme condition makes it medically necessary.
• Contacts.
- Contacts are covered if your vision cannot be corrected with glasses. Contacts
for convenience or cosmetic reasons are not covered. Cornea surgery for
myopia is not covered.
Wellness Exams for Adults
• Limited to once every 12 months.
• One screening mammogram per year for women over age 40.
Wellness Exams for Children
• Head-to-toe physical and developmental exams. The number of wellness exams a
child needs each year depends on the child’s age. All exams recommended by the
American Academy of Pediatrics are covered. It is important your children get
wellness exams according to the following schedule:
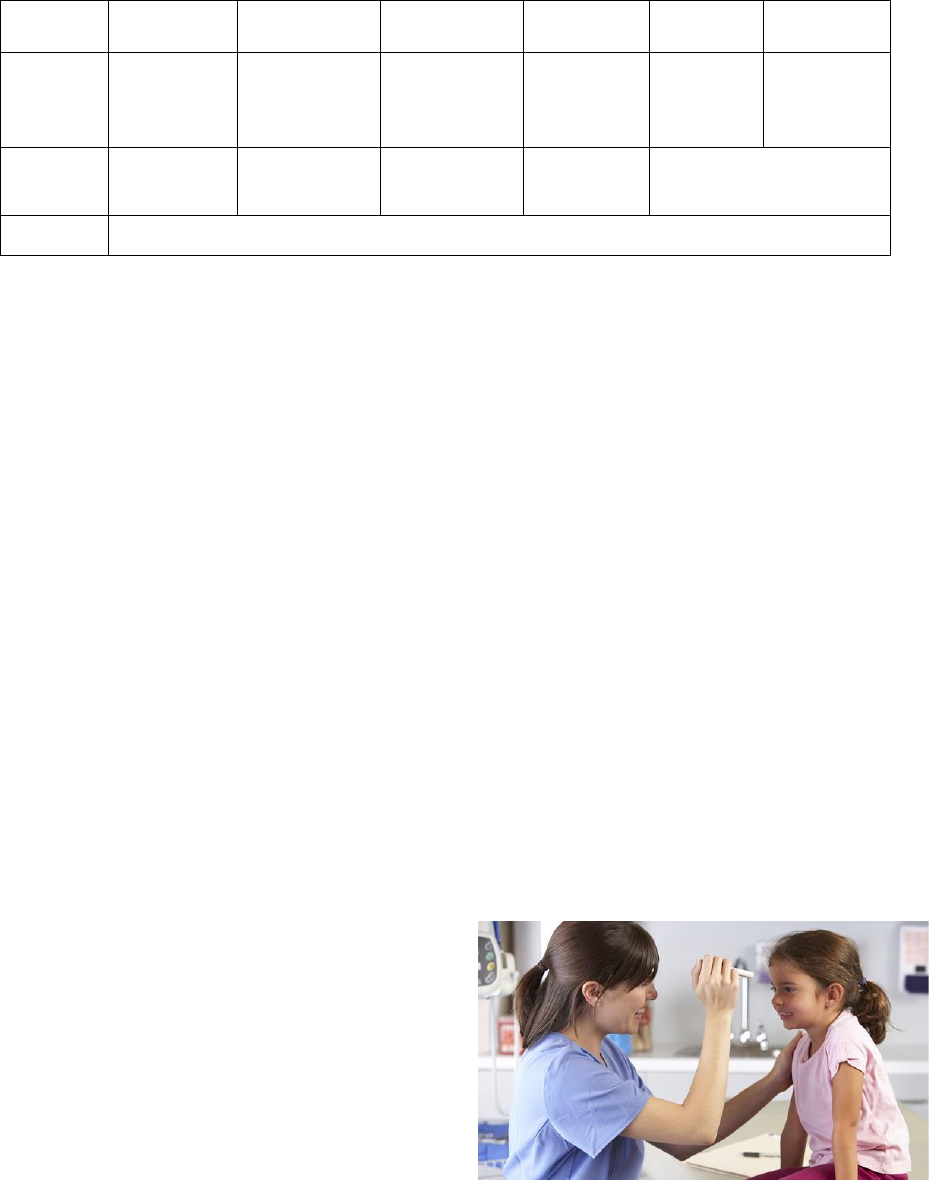
16
Child Wellness Exams Schedule
Age
✓
✓
✓
✓
✓
✓
Babies
At 1 week
and 1
month
2 months
4 months
6 months
9
months
12
months
1-3 yrs
15
months
18 months
24 months
30
months
36 months
3-19 yrs
1 wellness exam every year
It is just as important to take your children for wellness exams as it is to take them to the
doctor when they are sick. Regular exams allow time for you, your child, and your child’s
doctor to get to know each other and address any health concerns you may have about
your child. They help your doctor find health problems early, so your child can be
treated before they get worse.
During a wellness exam your doctor should discuss any health concerns you have about
your child and do the following activities:
• Document the history of your child’s development and health.
• Do a physical examination including measuring your child’s height and weight.
• Discuss physical activity habits.
• Discuss eating or nursing habits.
• Screen for developmental and behavioral issues.
• Do age-appropriate vision, hearing, and dental screenings.
• Give any appropriate immunizations.
• Order any needed lab tests.
• Perform a lead test at 12 and 24 months or up to age 21 if recommended.
You will receive letters from Idaho
Department of Health and Welfare Division of
Medicaid to remind you to schedule your
child’s wellness exam. Remember, wellness
exams for your child and services your doctor
recommends during the exams are covered at
no cost to you.

17
Idaho Medicaid Health Plan - The Enhanced Plan
The Enhanced Plan is for people with disabilities or special health needs and people
over the age of 65. This plan includes all the benefits that are in the Basic
Plan, plus some additional benefits.
Here is a summary of the additional services you may be eligible for if you are on the
Enhanced Plan:
• Home and Community-Based
• Hospice
• Nursing Home
• Personal Care Services
• Service Coordination
Brief Description of the additional services available
through the Enhanced Plan:
Home and Community-Based
• Supportive services that help people live in their home or
community rather than in an institution.
• Transition services that help people move out of an
institution and into a home in the community.
• Home and Community-Based Services are available for:
- Children with developmental disabilities.
- Adults with developmental disabilities.
- Children with serious emotional disturbance (SED).
- Adults who are elderly or have a physical disability.
Hospice
• In-home care for the terminally ill with six months or less to live.
Nursing Home
• Covered if your doctor says you need to be in a nursing home and Medicaid
determines that you need nursing home level of care.
18
Personal Care Services (PCS)
• Services provided in your home.
- Help people live more independently and have a better quality of life.
- Limited to 16 hours a week.
- If your medical condition requires more than 16 hours a week, you might be
eligible for one of the Home and Community-Based Waivers for adults or
EPSDT services for children and young adults under age 21 years.
Service Coordination
If you qualify for service coordination, you will have a service coordinator to help
you gain access and coordinate your necessary care and services. You can only
have one kind of service coordination. If you qualify for more than one kind, you
must choose the kind you want. The kinds of service coordination are:
• Targeted service coordination.
- For adults age 18 years old or older with a developmental disability.
- Requires prior authorization.
• Transition management.
- Transition management provides relocation assistance and intensive service
coordination activities to assist participants residing in a qualified institution
to transition to a community setting of their choice.
- A participant is eligible to receive transition management when planning to
discharge from a qualified institution after living within that institution for a
minimum of 45 Medicaid-paid days.
- Qualified institutions include the following; skilled, or intermediate care
facilities; nursing facility; intermediate care facility for persons with
intellectual disabilities; hospitals; and institutions for mental diseases.
• Children with special healthcare needs.
- Children up to age 21 years.
- Must have a medical condition that requires the child to be seen by many
service providers.
- An assessment and service coordination plan must be developed before
coordination services can be provided.
- Service coordination services are based on the service coordination plan and
must be prior authorized. If your child is age 0-3 years, the service
coordination agency must work with the Idaho Infant Toddler Program. You
can contact them at 888-535-0957.
• Outpatient behavioral health services.
- Care coordination services for children with serious emotional disturbance
(SED). See Behavioral Health.
- If you are under age 21 years, you can get additional services if your doctor
says they are medically necessary and they are prior authorized by Medicaid.
See Early and Periodic Screening, Diagnostic, and Treatment (EPSDT).
19
Idaho Medicaid Health Plan - The Medicare-Medicaid Coordinated Plan
The dual eligible plans are available if you qualify for both Medicaid and Medicare. To
better serve dual eligible participants, Idaho operates two different managed care
programs. The plans that are available are:
• The Medicare-Medicaid Coordinated Plan (MMCP) – a voluntary program
that is available in most Idaho counties. The Medicare-Medicaid Coordinated Plan
integrates all Medicaid and Medicare Part A, B, and D benefits into one plan.
• Idaho Medicaid Plus (IMPlus) - a mandatory program in certain Idaho counties
if you are eligible for both Medicare and Medicaid and have not enrolled in the
Medicare-Medicaid Coordinated Plan. The IMPlus coordinates Medicaid benefits for
people eligible for both Medicaid and Medicare who choose to have their Medicare
benefits administered through a separate plan.
You can participate in these plans if all the following apply:
• Over age 21 years
• Enrolled in Medicare Parts A and B
• Enrolled in the Medicaid Enhanced Plan
If you are eligible and choose to enroll, you
will have a care coordinator/specialist to
help you get the services that are right for
you. Available services include:
• Behavioral Health
• Durable Medical Equipment and
Supplies
• Home and Community-Based through the Aged and Disabled Waiver
• Hospital
• Personal Care Services
• Doctor and Specialist
• Prescription Drugs
• Skilled Nursing Facility
• Vision (not available for IMPlus plan)
The Medicare-Medicaid Coordinated Plan also offers some services that are over and
above original Medicare or Medicaid, including care coordination and access to a 24-
hour nurse advice line.
20
There is no premium or cost to join these
plans but if you currently have a share of cost
for waiver services or pay a premium for Part
D prescription drugs, these costs will not
change. These plans are managed through
Blue Cross of Idaho and Molina HealthCare of
Idaho.
If you would like more information about
these plans or would like to enroll, please
contact the Beneficiary Support Specialist at
833-814-8568 or [email protected].
Healthy Connections Primary Care Program
For those on Basic or Enhanced Medicaid,
Healthy Connections is a program that promotes
team-based care led by your primary care
provider and, most importantly, you! This section
will give you all the information you need about
the Healthy Connections program and how to get
more information if you still have questions.
What to Expect from Your Primary Care Provider
You can expect your primary care provider to:
• Provide your routine and preventive care.
• Coordinate your healthcare needs.
• Refer you to other healthcare specialists when needed.
Enrolling with a Primary Care Provider
Healthy Connections uses a fixed enrollment process. This means that once you are
enrolled with a primary care provider you will remain enrolled with that provider to
promote a quality, long-term relationship.
• Only you or your authorized representative can enroll or request a change in your
primary care provider.
• Once you are approved for Medicaid, you will receive a letter asking you to choose
your primary care provider.
• If you already have a primary care provider, please inform the Healthy Connections
program.
• Some providers choose to not participate in Healthy Connections or Idaho Medicaid.
You can search for providers here
https://www.idmedicaid.com/mhpviewer.aspx?FID=PDIR.
21
• If you need to find a primary care provider, a list of providers can be found here
healthyconnections.idaho.gov.
• You can submit your choice of Primary Care Provider by:
- Returning the enrollment form to Healthy Connections.
- Completing an enrollment form at your doctor’s office.
- Contacting Healthy Connections at 888-528-5861.
- Submitting your choice through the Live Better Idaho website at
https://www.livebetteridaho.org/.
• You will remain enrolled with your primary care provider unless you request a
change.
• You may choose to opt out of Healthy Connections if you are receiving Medicare,
foster care, adoption services, or are a member of a federally recognized tribe. To opt
out, you must contact Healthy Connections.
- Even though Medicaid does not require enrollment in Healthy Connections
under these scenarios, it may be a requirement of your clinic.
• Once you are enrolled, you will need to schedule an appointment to establish care
with your provider.
Changing your Primary Care Provider
• You can request a change to your primary care provider for any reason during the
annual enrollment period every January and February.
• You can request a change for any reason during the 90-day grace period after
enrollment to a new Healthy Connections provider.
• You would like to change between service locations within the same organization.
• You can request a change anytime if you meet one of the special circumstances
outlined in the section below.
• Once your change is approved, you need to sign a release of information at your new
provider’s office, so they can receive the records from your previous provider. This
will prevent disruption to your health services.
If you have questions about the program, need to find a primary care
provider, or need to change your primary care provider, contact
Healthy Connections at 888-528-5861 or visit the Healthy
Connections website at healthyconnections.idaho.gov.
22
Special Circumstances for Requesting a New Primary Care Provider
• You would like a different provider than the one
assigned to you by the Healthy Connections program,
as long as that assignment happened within the last 12
months.
• You moved and would like to select a primary care
provider closer to you.
• You would like to see a provider at the same Healthy
Connections clinic as another member of your
household.
• If for moral or religious reasons the primary care
provider does not cover the services you need.
• You need to change to or from a specialty provider (e.g., OB/GYN, pediatrics).
• You were placed in foster care.
• Your primary insurance coverage does not work with your current primary care
provider.
• If the provider decides the services you need are not available within the provider
network and it might put you at risk to obtain those services separately.
• If you want to follow your primary care provider to a different healthcare
organization and maintain your relationship with that provider.
• If the Department of Health and Welfare makes an administrative error.
The following three special circumstance requests must be submitted in
writing using our Special Circumstances form. You can get this form on the
Healthy Connections website at healthyconnections.idaho.gov.
• Receiving poor quality of care.
• A lack of access to covered services.
• A lack of access to providers experienced in dealing with your healthcare needs.
Referrals
A referral is your primary care provider’s approval for you to be
treated by another provider. You might not be able to get a
referral for other healthcare services if you have not seen your
primary care provider or if it has been more than a year since
your last visit. It is your responsibility to call your primary care
provider to find out if you need to be seen before a referral can
be made. It is important for you to:
• Tell your primary care provider about any medical services you need or have
received, such as emergency room visits and behavioral health services.
• Obtain a referral before you go to a provider who is not your primary care provider,
or you might have to pay the bill.
23
• If you are referred to another provider, contact them immediately to make an
appointment.
• Understand that an existing referral remains valid even if you change your primary
care provider.
You do not need a referral from your provider for:
• Acute medical services delivered in a
school-based health center
• Anesthesiology services
• Audiology services
• Children’s developmental disability
services
• Chiropractic services
• Dental services
• Durable medical equipment
• Emergency services
• Family planning services
• Home and Community Based Waiver
Services
• Hospice services
• Hospital admissions through the
emergency room
• Immunizations (without an office
visit)
• Intermediate care facility/
intellectually disabled (ICF/ID)
services
• Influenza shots
• Laboratory services (includes
pathology)
• Licensed midwife services
• Nursing facility services (including
services received outside the facility)
• Occupational therapy services
• Outpatient mental health services
• Personal care services
• Pharmacy services
• Physical therapy
• Podiatry services
• Pregnancy-related services
• Radiology services
• School district services
• Screening mammograms (40 or
older)
• Sexually transmitted disease testing
• Speech language pathology
• Substance use disorder services
• Transportation services
• Urgent care services
• Vision services
Note: Although you do not need a referral from your Healthy Connections provider to
receive these services, you may need to get a prior authorization. Please see page 27 for
more information about prior authorizations.
24
After-Hour Service
You can call your primary care provider 24-hours a day for information, referral, and
treatment for emergency medical conditions.
When to call the Healthy Connections Program: 888-528-5861
• If you need help choosing a primary care provider.
• If you want to change your primary care provider.
• If you are moving to a new area and need a new primary care
provider in that area. If you do not call when you move, you
will have to get a referral from your previous provider to get
care in your new area.
Your Role in the Healthy Connections Program
There are steps you can take to ensure your healthcare
needs are met and that you have the information and
access you need when you need it. These steps include:
• Calling your primary care provider when you need to
schedule an office visit, wellness exams, and anytime
you need medical advice, even after hours or on
holidays.
• Being on time to your appointments.
• Following your treatment plan.
• When you need to cancel your appointment, calling your primary care provider at
least 24-hours in advance when possible.
Note: Your provider can choose to stop providing care to you or a family
member if you miss appointments or do not follow your treatment plan.
• When you make an appointment or get care from any healthcare provider who bills
Medicaid, tell them you are enrolled in Healthy Connections.
• Showing your Medicaid card and any other insurance card at every appointment.
Note: Always show your Medicaid card and ask before you receive services if
they accept Medicaid for payment. Ask even when your doctor refers you to a
specialist, as not all doctors or healthcare providers accept Idaho Medicaid.

25
Healthy Connections Grievance Procedures
It is important that you know you can call the Healthy Connections program if you have
concerns or questions. If the Healthy Connections staff cannot fix the issue, you have the
right to file a written grievance. You can get the grievance form on the Healthy
Connections website at healthyconnections.idaho.gov.
Idaho Medicaid will review your grievance and provide a written response. If you are
still not satisfied, you have the right to file for a hearing. You can ask for a hearing by
writing directly to the address on your grievance response letter or sending your
grievance form to:
Department of Health and Welfare
Division of Medicaid
Healthy Connections Program
3232 Elder St.
Boise, ID 83705
Emergency Care
The emergency room or emergency department of a
hospital are not the places to get medical care unless it is
life-threatening. If you use them for routine medical care
you would usually get by visiting your primary care
provider, dentist, or specialty provider, you might be
charged a copayment (copay).
• Emergency rooms and ambulance services should only
be used when they are needed.
• You should always call your primary care provider for advice if you or a family
member gets injured or is sick.
• Your primary care provider can schedule an appointment or tell you if you need to
get emergency care.
• Your medical records from the emergency department will be given to your primary
care provider.
• If you visit the emergency room, you should make a follow-up appointment with
your primary care provider.
• Keep your Medicaid identification card with you so emergency personnel can better
treat you.
Crisis Services
• For immediate help, call 911 or go to the nearest hospital emergency room. You do
not need a prior authorization for help during a crisis.
• You can also contact 2-1-1 to help find services you need. The operators connect
people to many community resources.
• For a list of state crisis help lines, visit 2-1-1’s website at 211.idaho.gov or call 2-1-1.
• For the National Suicide Prevention Lifeline, call 800-273-8255 or 800-799-4889
(TTY).
26
Poison Control
If your child has swallowed a suspected poison or someone’s medication, call the
poison control center immediately at 800-222-1222 or 800-860-0620. Even
if your child doesn’t have symptoms of poisoning, they could be in danger.
Urgent Care
If your primary care provider’s office is closed or unable to see you immediately for an
urgent medical need, you can go to urgent care. Urgent care is a service that does not
require a referral or prior authorization. However, some medical services at urgent care
might require prior authorization.
• Be sure to show your Medicaid identification card and ask if it can be used as
payment.
• You should always call your primary care provider for advice if you or a family
member gets injured or is sick. Your primary care provider can schedule an
appointment or tell you if you need to get urgent care.
• You should see your primary care provider for all wellness exams, routine care, and
care for your chronic conditions.
Early and Periodic Screening, Diagnostic, and Treatment (EPSDT)
Medicaid pays for services that are medically necessary for children and young adults
under age 21 who are enrolled in the Basic or Enhanced plan offered by Idaho Medicaid.
EPSDT services include screening, preventive care, and diagnostic or treatment services
the child needs to lessen or correct physical or mental health conditions, even if the
service is not normally covered by an Idaho Medicaid Health Plan.
EPSDT services must be prior authorized.
Your provider must complete and submit a Request for Authorization packet. You can
download the packet from our website at
https://healthandwelfare.idaho.gov/Portals/0/Medical/MedicaidCHIP/EPSDTRequest
If you have questions about EPSDT or about completing the packet, please contact the
EPSDT Coordinator at 208-364-1165.
27
Prior Authorization
Prior authorization means you or your provider must obtain approval from Medicaid
before you get a service, or you might have to pay the bill.
Usually your doctor, healthcare provider, or pharmacist will request prior authorization
for you. You might have to request prior authorization for yourself or your family for
other services like transportation.
The following are examples of services that may need a prior authorization:
• Services that exceed limitations.
• Early and Periodic Screening, Diagnostic, and Treatment (EPSDT).
• Non-emergency medical transportation (NEMT).
• Some medical equipment and supplies.
• Some inpatient and outpatient hospitalizations or medical procedures.
• Some vision.
• Personal care services.
• Private duty nursing.
• Some prescription drugs and most brand name drugs when generics are available.
• Developmental disability agency services.
• Home and Community-Based Waiver services.
• Some laboratory and radiology.
• Outpatient behavioral health services may require prior authorization.

28
What Do I Need to Know About Paying for Services?
Copayments
• A copayment is a low fee that some providers might charge for some routine, non-
emergency services. If a doctor decides you need emergency treatment, you will not
have to pay a copayment for any of the services that are used during that treatment.
• If you have a copayment, the amount will depend on your age, your income, and
other factors. The department will let you know if you must pay a copayment and
how much you will have to pay.
You might need to pay a copayment for:
• Using the emergency room when it is
not an emergency
• Using emergency medical
transportation when it is not an
emergency
• Chiropractic care
• Doctor and healthcare provider visits
• Occupational therapy
• Physical therapy
• Podiatry
• Speech therapy
• Vision
Additional Information About Payment for Services
• If a doctor decides you need emergency treatment, you will not have to pay a
copayment for any of the services used during that treatment.
• If you are on the Aged and Disabled Waiver or the Adults with Developmental
Disabilities Waiver, you might be required to pay a copayment for the services you
receive under the waivers each month. This is called your “share of cost.”
• If you have a share of cost, you will be notified by the Idaho Department of Health
and Welfare. You will have to pay this amount directly to your waiver service
provider each month.
• You only pay a monthly share of cost toward the actual cost of waiver services you
use. If your calculated share of cost is higher than the cost of your services, you only
pay the lesser amount to your waiver provider.
• Share of cost only applies to waiver services. It does not apply to other Medicaid
services.
Before you start seeing providers, it is important that
you understand what you might need to pay for and
why. The information in this section will answer
questions you might have about copayments,
premiums, and why Medicaid might not pay for some
services. Providers must accept Medicaid’s payment as
payment in full except what’s listed below. They
cannot charge you for a “remaining balance.”
29
No Show or Missed Appointments
You are responsible for making and keeping
appointments. Your healthcare provider cannot charge
you a fee for missing appointments, but they can
decide to no longer see you as a patient.
Premiums
A premium is your monthly bill. Premium amounts are
determined by your income, and typically range from
$0 to $15. Department of Health and Welfare will send you a letter with your monthly
premium amount. You might need to pay a premium if:
• Your child is on the Basic Plan.
• Your child qualifies for the Home Care for Certain Disabled Children Program (Katie
Beckett) – premiums for these children are suggested and voluntary. If you are
unable to pay the premium amount, your child’s Medicaid eligibility will not be
affected.
• Your child with serious emotional disturbance is participating in the Youth
Empowerment Services (YES) program.
• You are participating in the Medicaid for Workers with Disabilities program.
For complete information about premiums, refer to the Medicaid public schedule of
premiums and cost sharing at
https://healthandwelfare.idaho.gov/Portals/0/Medical/MedicaidCHIP/PublicSchedule
OfPremiumsAndCostSharing.pdf.
Non-Covered Services
There are certain services that Medicaid does not pay for under certain circumstances,
including the following:
• Non-covered services or services excluded from coverage
You are responsible for the cost of an item or service that is not covered by Medicaid.
Before receiving the service, your healthcare provider should inform you that it is not
covered and tell you what your cost is if you decide to receive it.
• Care you receive from a provider who is not an Idaho Medicaid provider
Whether you receive care in Idaho or another state, Idaho Medicaid will not cover
the services you receive if the provider is not an Idaho Medicaid provider. It is your
responsibility to ask if the provider you are receiving services from is an Idaho
Medicaid provider. Providers who are enrolled in the Optum Idaho provider network
can provide behavioral health services.
• Care you receive without a Healthy Connections referral
Medicaid will not pay for care that requires a Healthy Connections referral if you do
not get a referral before receiving the care. Once you are approved for Medicaid,
you will receive a letter asking you to choose your primary care provider. You can
complete a Healthy Connections enrollment form at your primary care clinic. If you

30
do not choose a primary care provider, one will be assigned to you. Your Healthy
Connections primary care provider must know about any health conditions you
might have to make the right referrals for your care. It is your responsibility to call
your Healthy Connections primary care provider and ask whether you need to be
seen before you can obtain a referral. Your health plan may not pay for some services
without a referral.
• Care you receive without a prior authorization
Medicaid does not pay for care that requires a prior authorization if you do not get
the prior authorization before receiving services.
What Other Information Do I Need to Know?
Other Medical Insurance
If you have Medicare, Blue Cross, Blue Shield, or any
other medical insurance, tell your Department of Health
and Welfare benefits representative. Your other
insurance must pay before Medicaid will pay. If your
insurance has changed or stopped, please give your
Department of Health and Welfare benefits
representative your new insurance plan information or
say why you stopped your insurance. If you do not, you
or your children might not be able to get Idaho
Medicaid’s health insurance plan coverage.
If your primary insurance ends or changes, call 208-375-1132, option 3, or toll
free at 800-873-5875. For more information about benefits, call 866-686-4752.
If Medicaid pays a bill and you get money from your other insurance, you are required
to give the money to Medicaid. You are responsible for helping Medicaid collect money
from another insurance plan or a responsible person such as a non-custodial parent.
The provider of the services will need to re-bill or do an adjustment.
For instructions about how to pay Medicaid, call the Financial Recovery Unit at
208-287-1152 or the Department of Health and Welfare’s third-party recovery
contractor (HMS) in the Boise area at 208-375-1132, or toll free at 800-873-5875.
Health Insurance Premium Payment Program
If you have Medicaid and have other health insurance available, such as employer-
sponsored group coverage, ask your Department of Health and Welfare representative
about this program. If you or your children qualify, the Department of Health and
Welfare may pay the premiums, deductibles, and copayments for your other insurance.

31
Your Rights
When you are eligible for Idaho Medicaid’s health
insurance coverage, you have certain guaranteed rights.
These include:
• You have the right to fair treatment. You have
the right to all covered benefits without regard to race,
color, national origin, religion, disability, sex, or age.
You have the right to be treated with respect and with
due consideration for your dignity and privacy. You
have the right to be free from any form of restraint or
seclusion used as a means of coercion, discipline, convenience, or retaliation.
If you believe that anyone in the Department of Health and Welfare has
discriminated against you because of your race, color, national origin, religion,
disability, sex, or age, you can file a complaint by contacting:
Civil Rights Manager
Idaho Department of Health and Welfare
PO Box 83720
Boise, Idaho 83720-0036
208-334-5617 (voice) or 208-334-4921 (TDD)
You can also file a complaint by contacting:
U.S. Department of Health and Human Services (HHS)
Director, Office for Civil Rights
Room 506-F, 200 Independence Avenue, S.W.
Washington, D.C., 20201
202-619-0403 (voice) or 202-619-3257 (TDD)
• You have the right to timely and accurate notice. Written notifications must
be mailed to you before your eligibility is ended, so keeping your address up to date
is important.
• You have the right to receive information about available treatment
options. The information should be given to you in a manner that is appropriate to
your condition and ability to understand.
• You have the right to make decisions about your healthcare. Your provider
must discuss your options with you before you start medical treatment. You should
let your family and your doctor know your wishes before you become too ill to make
a decision about your medical treatment.
• You have the right to request and receive a copy of your medical records.
You can request that they be amended or corrected.
32
• You have the right to file an appeal.
For eligibility appeals, the Department of Health and Welfare must
receive your appeal in writing within 30 days from the date the notice
was mailed.
If you disagree with a decision regarding your eligibility coverage, or if you feel
that your medical needs have not been properly met, you can file an appeal or
request a Fair Hearing Form at your local Health and Welfare Office or by calling
877-456-1233.
For managed care service and benefits appeals. The managed care
contractor must receive your appeal request within 60 days from the
date on the notice.
If you disagree with a decision made regarding your service and benefits provided
by one of Idaho Medicaid’s managed care partner, you must first file your appeal
with the contractor as outlined below:
Behavioral Health services
Optum Idaho
205 East Watertower Street
Meridian, ID 83642
Fax: 855-272-7053
Phone: 855-202-0973
Dental services
MCNA Dental
Attn: Grievances and Appeals Department
200 West Cypress Creek Road, Suite 500
Fort Lauderdale, FL 33309
Fax: 954-628-3330
Phone: 855-233-6262
Appeal form:
http://docs.mcna.net/forms/id-member-
appeal
Dual Eligible, Medicare-
Medicaid Coordinated services
If you want to appeal a decision about your
dual eligible benefits, call the number on the
back of the healthcare card you receive from
your health plan or call your care
coordinator.

33
Transportation, Non-Emergency Medical Transportation (NEMT).
The NEMT contractor must receive your appeal request within 28
days from the date on the notice.
If you disagree with a decision made by MTM, you can file an appeal, grievance,
or a state fair hearing request. You can do this by calling or writing to us within
28 days of the date on your denial letter.
MTM
Attn: Appeals
16 Hawk Ridge Drive
Lake St. Louis, MO 63367
Phone: 866-436-0457
State Fair Hearing - Medicaid services and benefits. For Medicaid
appeals, the Department of Health and Welfare must receive your
appeal in writing within 28 days from the date the notice was mailed.
If you disagree with a decision made regarding your service or benefits provided
by Idaho Medicaid, you must file your appeal in writing within 28 days from the
date the notice of decision was mailed as outlined below.
You can submit your written appeal in-person to your regional office or send it by
mail, e-mail or fax to the following:
Medicaid Appeals
Idaho Department of Health and Welfare
PO Box 83720
Boise, Idaho 83720-0009
Fax: 208-364-1811
Email: [email protected]
If a hearing is scheduled, you will receive a notice of scheduling letter with the
date and time of your hearing. During the hearing, you can have anyone you want
present to speak on your behalf, if they are an authorized representative. If you
decide you want an attorney to represent you, you are responsible for any fees.

34
Fraud, Abuse, and Misuse
Everyone in your family eligible for health benefits will
get their own Medicaid card with their name listed on the
card. It is against the law for anyone else to use the card.
If you knowingly break the rules, you can lose your
coverage. You also can be prosecuted, and you might have
to pay for the benefits you received but were not entitled
to receive.
If you think someone receiving assistance from the state
of Idaho is abusing the programs or you think a provider is improperly billing for
services they have not provided, you should report this to Medicaid.
• To report member fraud, call the Idaho CareLine at
2-1-1 or 800-926-2588.
• To report provider fraud, download the complaint form from
http://healthandwelfare.idaho.gov/Portals/0/Mgmt%20Services/Provider%20Frau
d%20Complaint%20Form.pdf. Fill out the form and mail it to:
Medicaid Fraud & Program Integrity Unit
Bureau of Audits and Investigations
PO Box 83720
Boise, Idaho 83720-0036
Fax: 208-334-2026
Estate Recovery
Medicaid estate recovery is the process through which each state recovers the costs of
medical services it has paid from the estate of the person who received those services.
The Medicaid estate recovery program impacts two groups of people receiving Medicaid
benefits:
• Anyone over the age of 55 who has received Medicaid assistance, and
• Anyone who is permanently institutionalized and has received Medicaid assistance,
regardless of age.
The estate recovery program may collect money from the estate of a deceased Medicaid
recipient as repayment for any medical care services that were provided to the recipient
and paid for by Medicaid, while the recipient was over 55 years of age, or permanently
institutionalized, regardless of age.
Medical care includes a wide range of services, including nursing home and community
based in-home care services. It also includes any hospital and prescription drug services
the participant received while in a nursing home, or while receiving in-home
care. Medical care also includes capitation payments to Medicaid contracted health
insurance companies or medical providers administering a defined package of benefits.
The federal government directs states to pursue Medicaid estate recovery for these
services.
35
Federal law recognizes that the needs of certain relatives can take precedence over the
state’s interest in recovering assets from the deceased. For this reason, states are not
allowed to pursue Medicaid estate recovery under the following circumstances:
• During the lifetime of the surviving spouse, regardless of where he or she lives.
• From a surviving child who is under age 21 years or is blind or permanently disabled
(based on Social Security criteria), regardless of where he or she lives.
As individual circumstances vary, and for more information, please call the Estate
Recovery Office at 866-849-3843.

36
Who Can I Call If I Have Questions or
Need Information?
Beneficiary Support Specialist (for
Dual Eligible Plans)
833-814-8568
Customer Service Line and
Application Processing Center
You can call 877-456-1233 to apply or
get help at any Self-Reliance Office.
Mail: Department of Health and Welfare
PO Box 83720
Boise, Idaho 83720-0036
Dental Coverage – Idaho Smiles
For information about dental coverage
or to find a dentist in your area, contact
MCNA Dental at 855-233-6262 or visit
MCNA’s website at
https://www.mcnaid.net/en/find-
dentist.
Disability Coverage for People
Over 65 years old
If you are over 65, receiving Social
Security benefits due to disability, or if
you are applying for Medicaid for an
elderly person with a disability, please
call the customer service line toll free at
877-456-1233.
Estate Recovery Office
To find out about estate recovery, call
866-849-3843.
Families with Children
For information or to find out about the
status of your application for Idaho
Medicaid’s health plan coverage, call the
customer service line toll free at
877-456-1233.
Fraud and Program Integrity
To report member fraud, call the Idaho
CareLine at 2-1-1 or 800-926-2588.
Health Management Systems
To report changes to your other
insurance, call the Department of Health
and Welfare’s third-party recovery
contractor (HMS) in the Boise area at
208-375-1132, or toll free at
800-873-5875.
Behavioral Health
To find a provider, contact Optum Idaho
at 855-202-0973 or visit Optum’s
website at
https://www.optumidaho.com/.
Idaho Department of Health and
Welfare’s Civil Rights Manager
If you feel that the Department of
Health and Welfare has discriminated
against you, call 208- 334-5617 (voice)
or 208-334-4921 (TDD).
Infant Toddler Network
Call 888-535-0957.
Medicare
For more information about Medicare,
call 800-MEDICARE (800-633-4227) or
visit Medicare’s website at
https://www.medicare.gov/.
Non-Emergency Medical
Transportation
To request transportation through
Medicaid’s non-emergency medical
transportation provider, MTM, call
877-503-1261 or visit MTM’s website at
https://www.mtm-inc.net/idaho/.
37
Nursing Home Assistance/Long-
Term Care Unit
For information about nursing home
assistance or the status of your
application for nursing home assistance,
call the Long-Term Care Unit toll free at
866-255-1190. Fax 208-799-5048.
U.S. Department of Health and
Human Services (HHS)
202-619- 0403 (voice) or
202-619-3257 (TDD)
Help with Other Services
To get help with other services available
through the Department of Health and
Welfare, call the Idaho CareLine (2-1-1
or 800-926-2588) or call
877-456-1233.
Help with Your Covered Services
If you have questions about your
covered services, please call the DXC
Member line at 866-686-4752.
Reasons you might call the DXC
member line include:
• If a doctor or medical service
provider reports you to a collection
agency or if you get a bill that you
think your health plan should pay.
• If you want to know whether a
service needs a Healthy Connections
referral or prior authorization.
• If you need to know whether an item
or service is covered.
• Do not call the Member line for
eligibility questions; instead
contact the customer service line toll
free at 877-456-1233.
38
Local Healthy Connections Offices
Local offices can tell you about available primary
care providers in your area and help you with
changes or questions about Healthy Connections.
For more information, please visit the Healthy
Connections website healthyconnections.idaho.gov.
Healthy Connections Customer Service
Toll-free: 888 528-5861
Español: 800-378-3385
Fax: 888-532-0014
Email: [email protected]
Region 1 – Coeur d’Alene
Benewah, Bonner, Boundary, Kootenai, and Shoshone counties
1120 Ironwood Dr., Suite 102
Coeur d’Alene, Idaho 83814
208-666-6766
Region 2 – Lewiston
Clearwater, Idaho, Latah, Lewis, and Nez Perce counties
1118 F St.
Lewiston, Idaho 83501
208-799-5088
Region 3 – Caldwell, Nampa, & Payette
Adams, Canyon, Gem, Owyhee, Payette, and Washington counties
3402 Franklin Rd.
Caldwell, Idaho 83605
or
515 N. 16
th
St.
Payette, Idaho 83661
208-642-7006
Region 4 – Boise
Ada, Boise, Elmore, and Valley counties
1720 Westgate Dr.
Boise, Idaho 83704
208-334-4676
Region 5 – Twin Falls & Burley
Blaine, Camas, Cassia, Gooding, Jerome, Lincoln, Minidoka, and Twin Falls counties
601 Pole Line Rd., Suite 3
Twin Falls, Idaho 83301
208-736-4793
39
Region 6 – Pocatello
Bannock, Bear Lake, Bingham, Caribou, Franklin, Oneida, and Power counties
1090 Hiline Rd., Suite 202
Pocatello, Idaho 83201
208-235-2927
Region 7 – Idaho Falls
Bonneville, Butte, Clark, Custer, Fremont, Jefferson, Lemhi, Madison, and Teton
counties
150 Shoup Ave., Suite 4
Idaho Falls, Idaho 83402
208-528-5794

40
Regional Program Offices
Local offices help with developmental disability service applications, home and
community-based waivers, assessments for personal care services, and children’s
services.
Region 1 – Coeur
d’Alene
1120 Ironwood Dr.
Coeur d’Alene, Idaho 83814
208-769-1567
Region 2 – Lewiston
1118 F St.
Lewiston, Idaho 83501
208-799-4430
Region 3 – Caldwell
3402 Franklin Rd.
Caldwell, Idaho 83605
208-455-7150
Region 4 – Boise
1720 Westgate Dr.
Boise, Idaho 83704
208-334-0940
Region 5 – Twin Falls
601 Pole Line Rd., Suite 3
Twin Falls, Idaho 83301
208-736-3024
Region 6 – Pocatello
1070 Hiline Rd.
Pocatello, Idaho 83201
208-239-6260
Region 7 – Idaho Falls
150 Shoup Ave., Suite 4
Idaho Falls, Idaho 83402
208-528-5750
