Transformational Leadership
Strategic Planning (1)
1
Strategic Planning
Source of Evidence 1
Describe and demonstrate how nursing’s mission, vision, values, and strategic and quality
plans reflect the organization’s current and anticipated strategic priorities.
Context for Vanderbilt Nursing Mission, Vision, Values and Strategic Plans
Vanderbilt is a complex academic medical center. The detail about the organizational
structure is comprehensively reviewed in Organizational Overview 1 however, there are some
important organizational relationships to consider related to alignment of mission, vision and
strategic and quality plans. Vanderbilt University Medical Center is comprised of four entities.
These include Vanderbilt University Hospital, The Monroe Carell Junior Children’s Hospital,
Vanderbilt Psychiatric Hospital and the Vanderbilt Medical Group and Clinics and all are part of
the Vanderbilt Magnet designation. The Chief Executive Nursing Officer provides leadership for
the provision of nursing care across all of these entities. Thus, the nursing mission, vision and
strategic plan must be relevant in each of the entities. An extremely important strategic alliance
is with the Vanderbilt Medical Group which is the physician practice portion of the organization.
Alignment of physician and nursing professions within each entity is critical to maximizing
patient outcomes.
This source of evidence demonstrates the alignment of the nursing mission, vision,
values and strategic plan within the context of the broader organization and within the
Vanderbilt Medical Group. The CEOs of the entities described above as well as the Executive
Chief Nurse report as peers to the to the Vice Chancellor of Health Affairs and thus have equal
influence over the organization’s strategic and quality plans.
Nursing and the Organization Vision and Mission Alignment
Vanderbilt provides us a stimulating, intellectually rich and supportive environment to
develop the science and art of nursing and to bring the full potential of nursing practice to bear
on patients and families. The mission, vision and values of nursing are driven by the philosophy
of nursing represented in Table TL 1-1 as well as the principles set forth in the Vanderbilt
Nursing Bylaws Table TL 1-2. (Complete copy of Nursing Bylaws in OO 3). The content of these
foundational documents ensure that nursing is clear in its focus for strategic planning and
integrates within a complex organization. Fully grounded in a deep understanding of, and
Transformational Leadership
Strategic Planning (1)
2
commitment to the discipline of nursing, the profession of nursing at Vanderbilt is leading the
way in innovation and excellence. To that end, the nursing vision, mission and values have been
developed and then integrated into the strategic vision and planning for Vanderbilt University
Medical Center.
The CNO is engaged and involved in the planning process for the system and brings the
message of professional nursing to the executive table. Likewise nurses across the organization
in all roles and all settings are part of the planning and implementation of this strategic vision as
they are included in many of the planning and implementation teams. (Committee information
in OO 15) It is this process of matrix decision making and inclusion of all disclilpines in clinical
testing of new ideas and processes to improve patient care that makes Vanderbilt a system that
continues to grow, and strive to meet all aspects of its mission and vision.
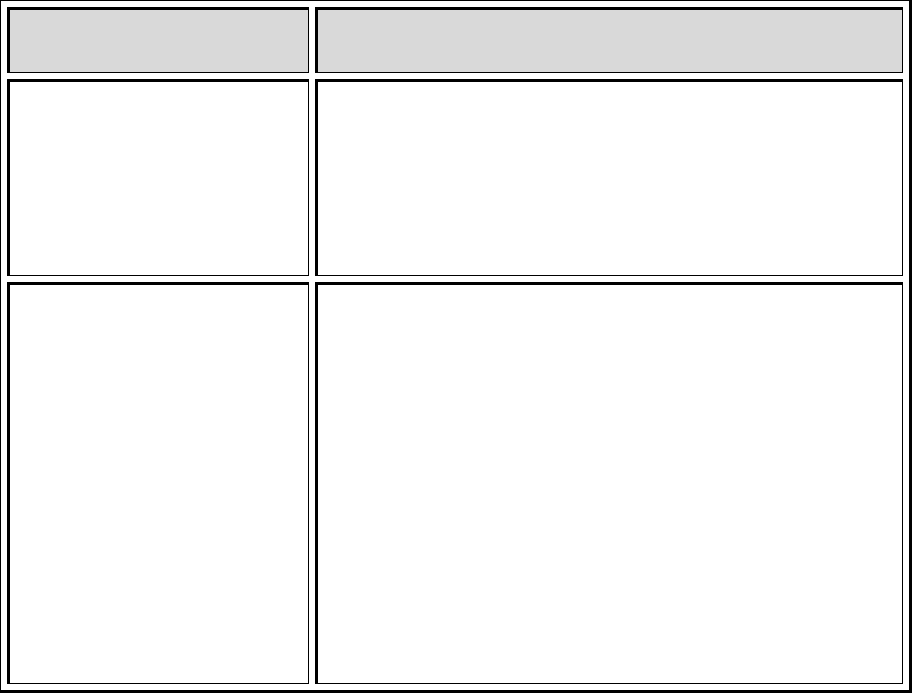
Table TL 1-3 demonstrates the relationship between the University mission statement,
the Medical Center mission statement, The Vanderbilt Medical Group and the nursing mission
statements. The process of strategic planning for nursing and the organization is reviewed in
TL3.
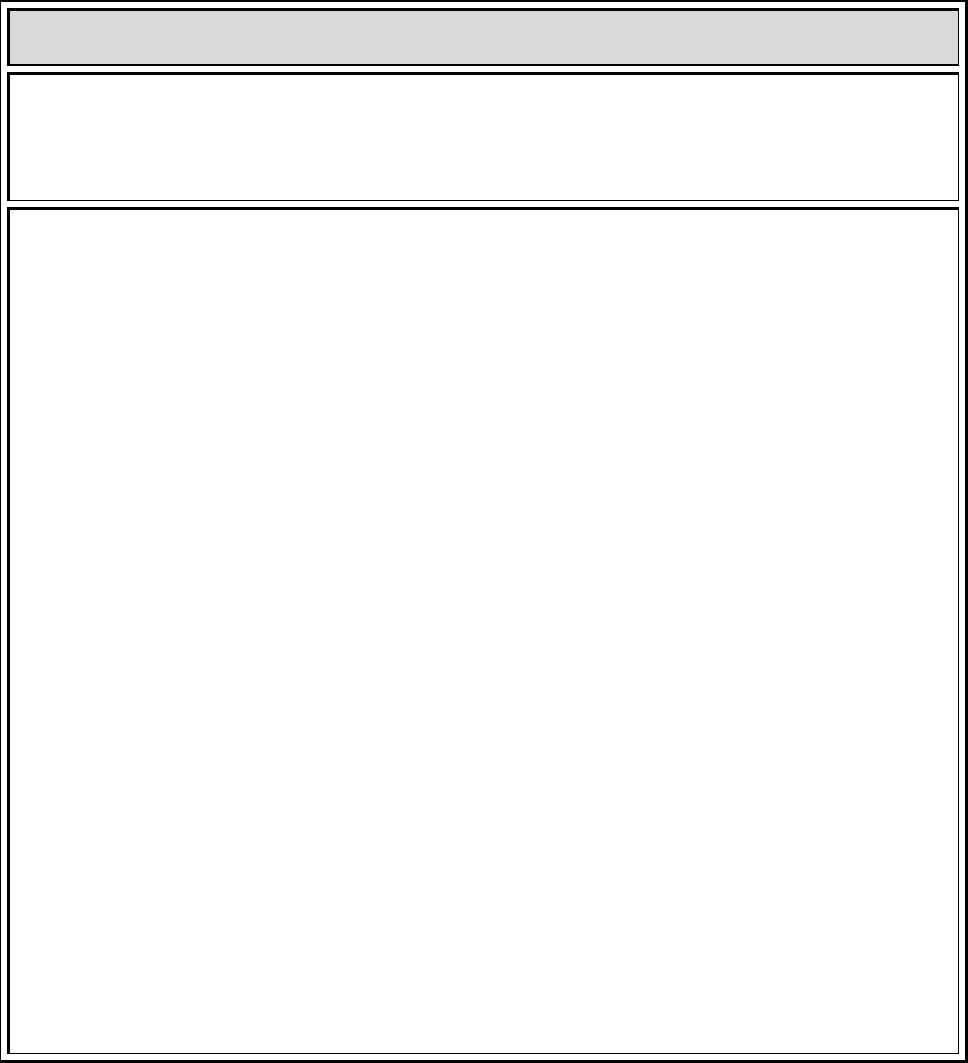
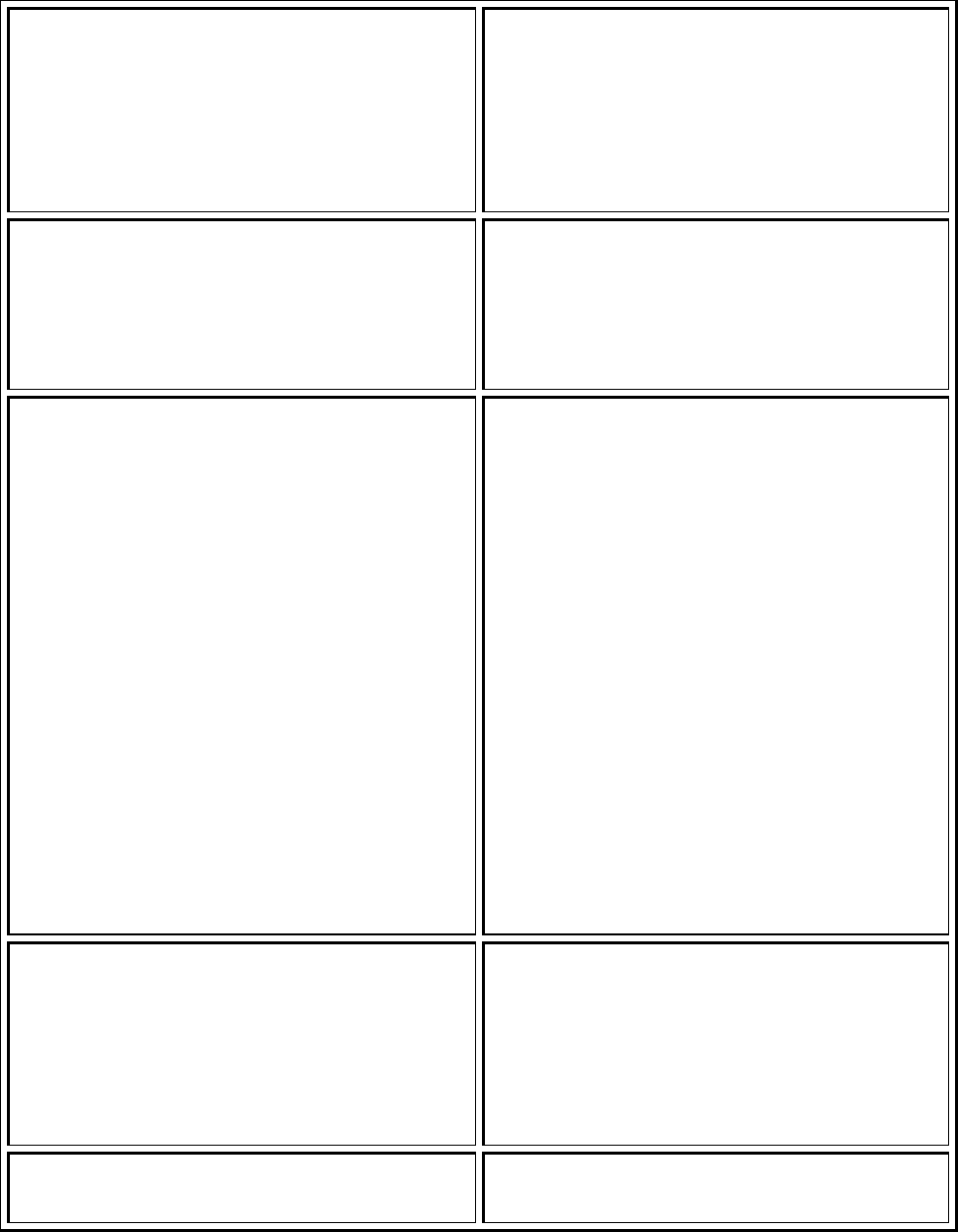
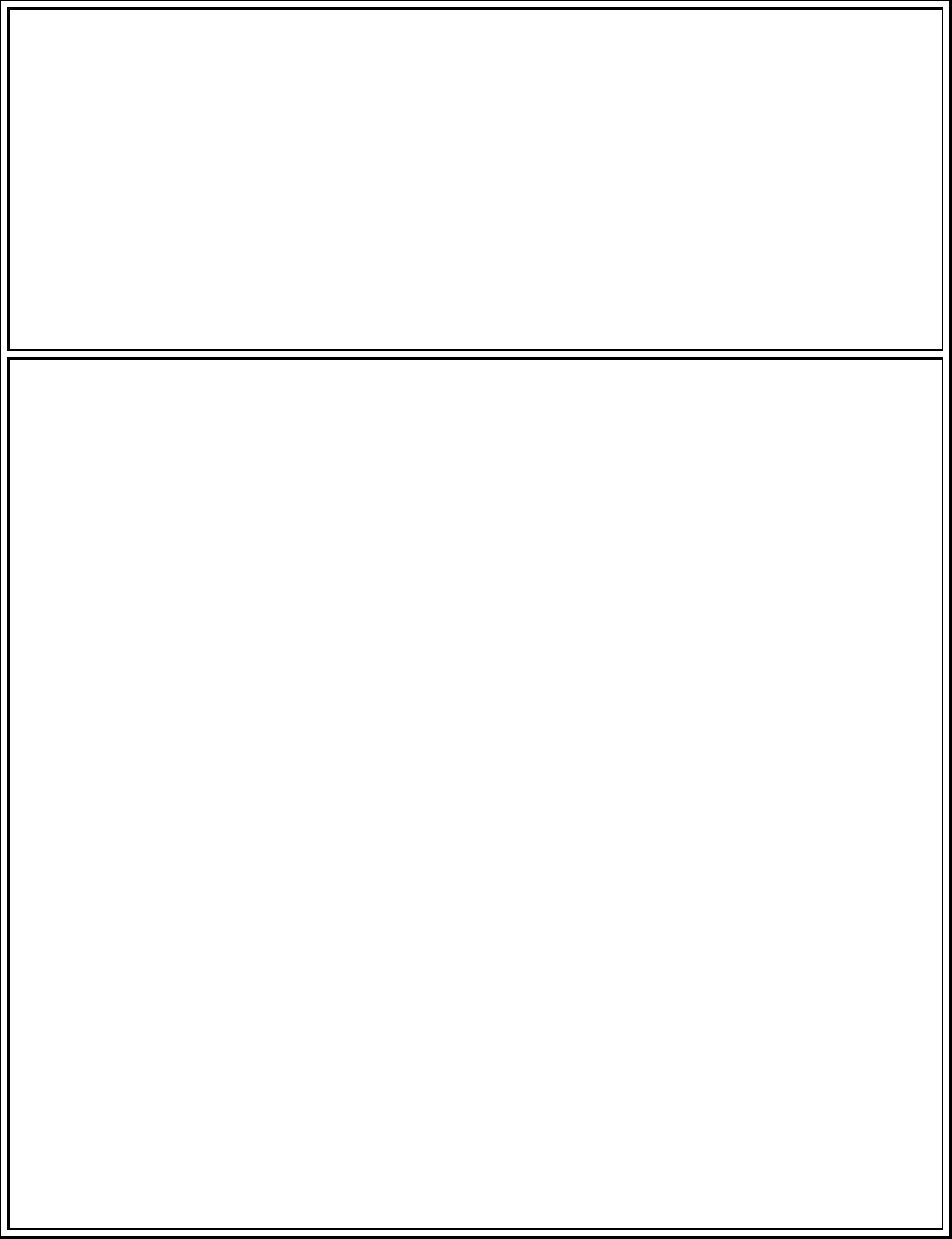
Table TL 1 – 1: Philosophy of Nursing
PHILOSOPHY OF NURSING
VANDERBILT UNIVERSITY MEDICAL CENTER
We believe that the provision of highly skilled and specialized nursing care is essential to the
fulfillment of Vanderbilt University Medical Center’s mission of improving health care outcomes
through quality in patient care, education and research. Nursing embraces the responsibility to
provide patient centered, high quality, and cost effective nursing care for all patients and their
families.
We believe nursing is an applied art and science with the focus of professional practice being to
assist individuals, families and communities in achieving optimum health and well-being. This
assistance includes preventive health care, education, facilitating recovery and continued
support through illness, disability, or death. Professional nurses collaborate with physicians and
other disciplines to deliver coordinated and comprehensive patient care. This collaborative care
takes place in a variety of settings.
We are guided by a philosophy that recognizes the inherent worth, dignity and uniqueness of
every individual. We promote participation of patients and significant others in decisions
regarding the patients’ health care and work toward their optimal level of wellness.
Transformational Leadership
Strategic Planning (1)
3
We are committed to providing an environment that continually seeks to improve delivery of
patient care, facilitates rapid changes in practice, and encourages flexibility throughout all
levels of care providers. We believe in the concept of Shared Governance whereby staff
participates in decisions affecting nursing practice and the clinical work environment. We
believe in the enhancement of an environment that fosters effective communication at all
levels, provides recognition of nursing staff for excellence in clinical practice and promotes the
recruitment and retention of clinically competent staff. We support the roles of nurses in
advanced practice as clinical experts and resources for the enhancement of patient care
throughout the care continuum.
We believe that research is a vital component for the advancement of evidenced-based clinical
practice. Systematic evaluation of the effectiveness of nursing practice contributes to the
improvement of patient care and the expansion of nursing knowledge. Excellence in nursing
practice is enhanced by creating an environment that provides opportunities for advanced
nursing education as well as stimulating personal and professional growth. We seek to foster
innovation by working collaboratively with other disciplines to develop new models of clinical
practice to improve quality patient outcomes.
We believe that the future of the profession rests upon developing collaborative models
between nursing service and nursing education. Nursing facilitates the education of patients,
families, nursing peers, colleagues from other disciplines and students of the various health
professions. Each nurse serves as a role model of quality professional practice.
We are accountable for our practice in accordance with recognized professional standards and
ethical codes. We accept the challenge of providing high quality nursing care as a member of
the total health care team in a complex and dynamic health care environment.
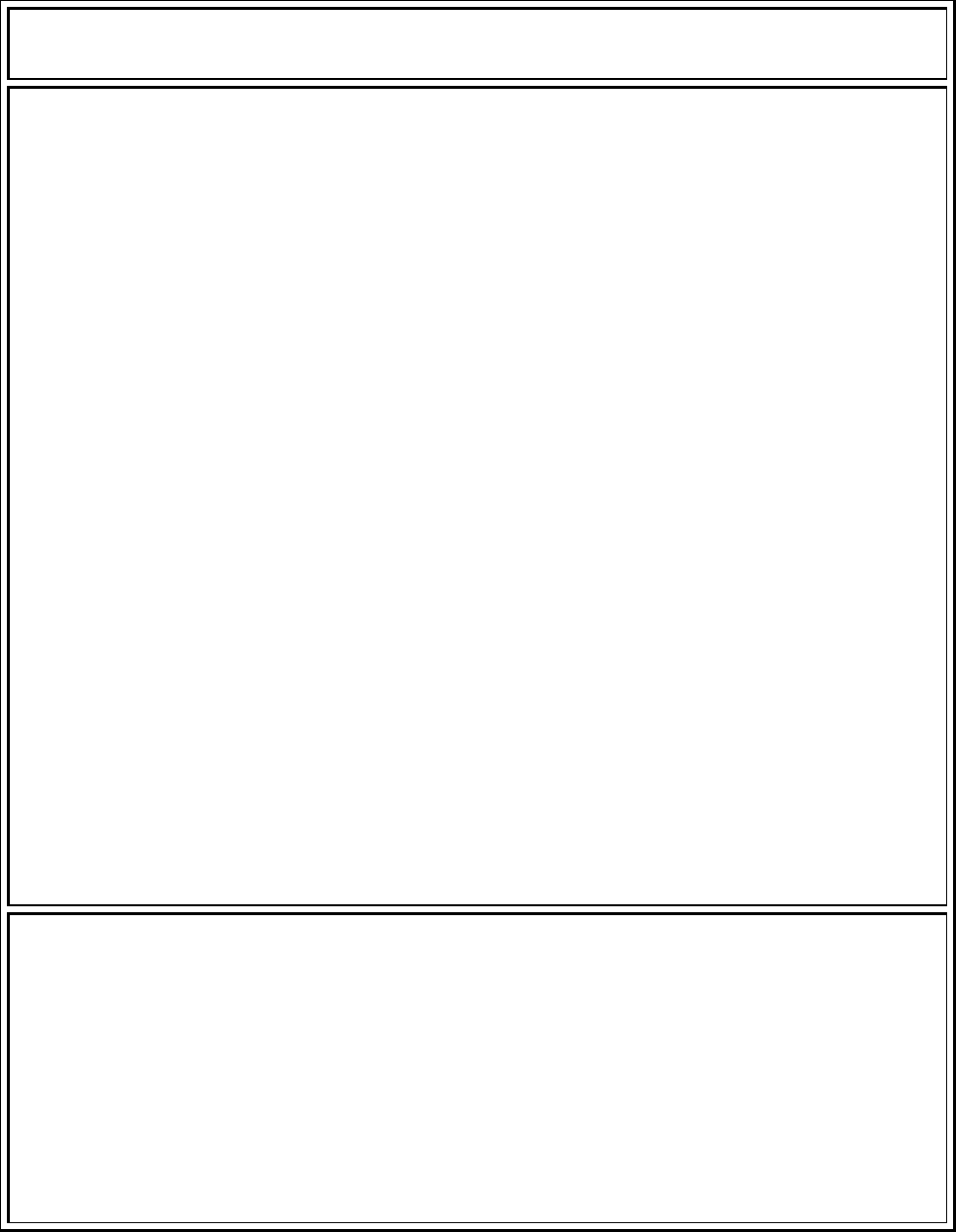
Table TL 1-2: Nursing Bylaws Preamble - below
Transformational Leadership
Strategic Planning (1)
4
Preamble to the Nursing Bylaws
The nursing staff of VUMC is responsible for the nursing care administered to our patients, with the
Board of Trust having the ultimate authority. In order to effectively fulfill this obligation, the nursing
staff conforms with the Bylaws, which are formulated upon the following principles:
1. All patients are entitled to safe, effective, evidence-based nursing care.
2. Nursing care of the patient is enhanced by use of an evidence-based care delivery system
tailored to the uniqueness of each patient and provider.
3. The continuing measurement, evaluation, and improvement of nursing practice are essential to
the provision of safe, effective, evidence-based nursing care.
4. The patient is best served by the nursing staff’s collaboration with other hospital staff,
participation in educational and research programs, and use of evidenced based practice.
5. All nursing staff is accountable for our mission of continuous quality improvement, patient
safety, customer satisfaction, and cost effective, evidence-based, value added care.
6. Patients are best served in a healthcare environment that fosters learning, stimulates
professional growth and promotes nursing research and innovation in nursing practice.
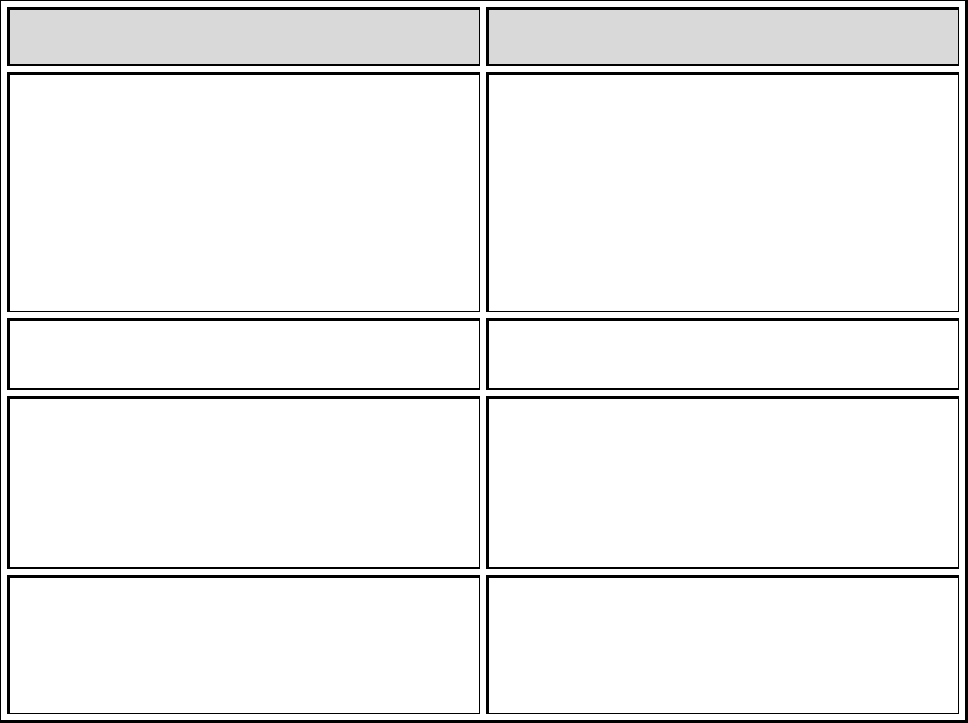
Table TL 1-3: University, Medical Center and Nursing missions, vision and values
Vanderbilt University
Mission
Vanderbilt Medical
Center Mission
The Vanderbilt
Medical Group and
Clinics
Vanderbilt Nursing
Mission, Vision and
Values
Vanderbilt University is a
center for scholarly
research, informed and
creative teaching, and
service to the community
and society at large.
Vanderbilt will uphold the
highest standards and be a
leader in:
the quest for new
knowledge through
scholarship,
dissemination of
knowledge through
teaching and outreach,
Creative
Vanderbilt University
Medical Center
(VUMC) is a
comprehensive
healthcare facility
dedicated to patient
care, research, and
biomedical education.
Its reputation for
excellence in each of
these areas has made
Vanderbilt a major
patient referral center
for the Mid-South.
Each year, people
throughout Tennessee
and the Southeast
MISSION
The Mission of
VMG is to improve
the health of the
people in the
communities we
serve through
evidence-based
personalized
compassionate care
research, ad
education.
VISION
The Vision of VMG
is to shape the
future of
MISSION
Advance health and
wellness through
excellence in nursing
care, education, and
research throughout the
lifespan and across the
continuum of care.
VISION
To be the national leader
in nursing practice,
education and research
in all nursing roles,
Transformational Leadership
Strategic Planning (1)
5
experimentation of
ideas and concepts.
In pursuit of these goals,
Vanderbilt values most
highly
Intellectual freedom
that supports open
inquiry, equality,
compassion, and
excellence in all
endeavors.
choose Vanderbilt for
their health care
needs, not only
because of its
excellence in medical
science, but also
because the faculty
and staff are
dedicated to treating
patients with dignity
and compassion.
Vanderbilt's mission is
to advance health and
wellness through
preeminent programs
in patient care,
education, and
research.
healthcare through
discovery and
innovation.
VALUES
We make those we
serve our highest
priority.
We respect privacy
and confidentiality
We communicate
effectively with our
patients and
colleagues
We conduct
ourselves
professionally, with
respect and
compassion.
We have a sense of
ownership for the
health of our
communities
We have a high
commitment to our
colleagues
specialties, and settings.
VALUES
We value:
patient safety and
quality
Having strong
interdisciplinary
collaboration and
communication.
having effective
shared decision
making
and support a
continuous learning
environment.
providing meaningful
rewards and
recognition
highly specialized
nursing care and
influencing the
nursing practice
patient and family
centered care
improving the health
of the community
through outreach,
research and
wellness initiatives.
Behavioral Alignment of Nursing and the Organization
An important part of the foundation for Vanderbilt that aligns nursing and all disciplines
is the Vanderbilt Medical Center Credo. The credo translates the mission and vision into
foundational behaviors for all faculty and staff. It is commonly referred to as describing “It’s
Who We Are”. Regardless of the role at Vanderbilt, all faculty, staff, nursing and other
disciplines, are held accountable through performance management for demonstrating
Transformational Leadership
Strategic Planning (1)
6
behaviors described by the credo. The credo provides consistency, accountability and a shared
understanding of behaviors that optimize patient outcomes and staff satisfaction. The Credo is
presented in Table TL 1-4.
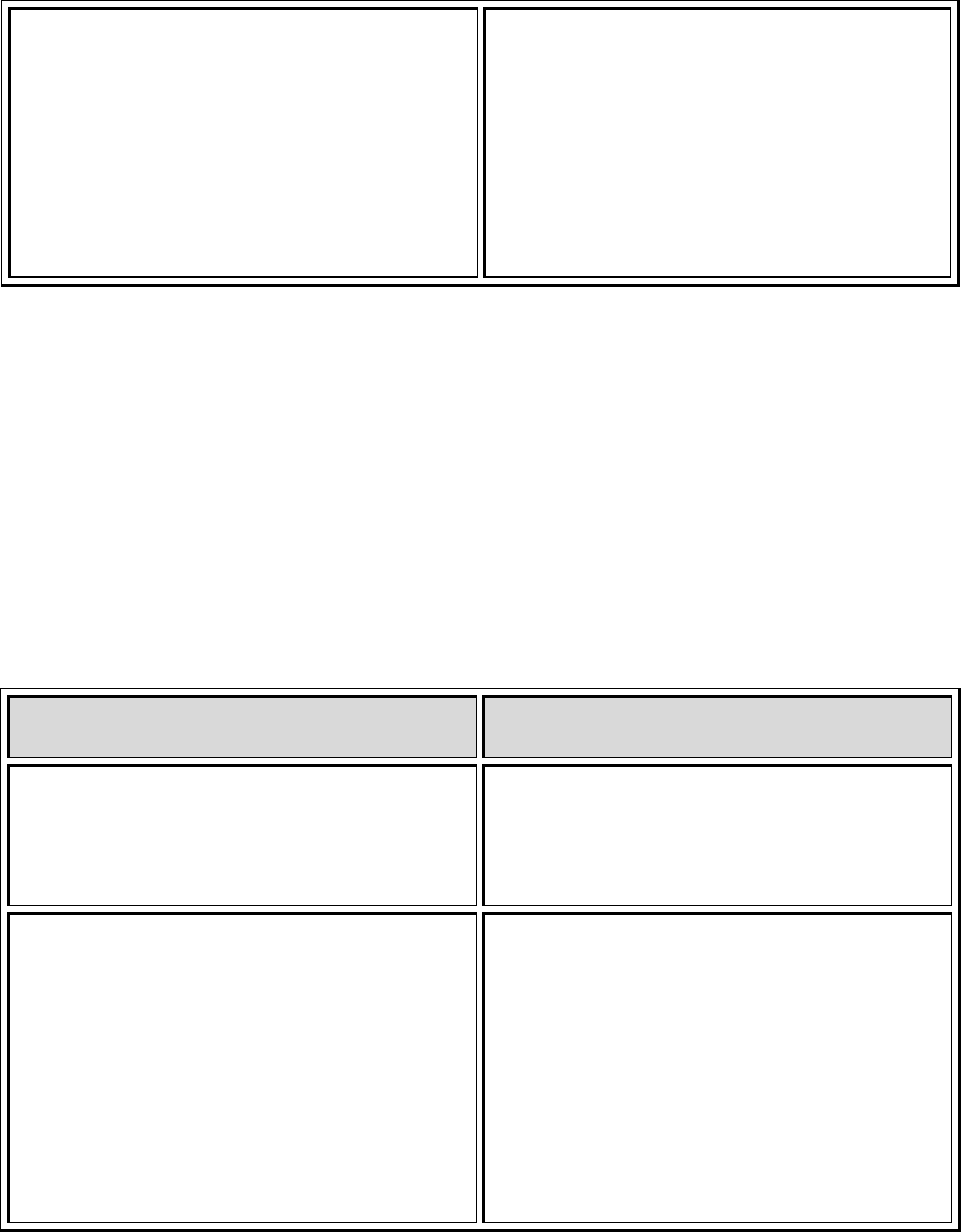
Table TL 1 – 4: VUMC Credo
Vanderbilt University Medical Center Credo
We provide excellence in healthcare, research and education.
We treat others as we wish to be treated.
We continuously evaluate and improve our performance
I make those I serve my highest priority:
• promote the health and well being of all patients who seek care at Vanderbilt
• support trainees in all of their academic endeavors
• respect colleagues and those we serve who differ by gender, race, religion, culture,
national origin, mental and physical abilities and sexual orientation and treat them with
dignity, respect and compassion
• recognize that every member of the Vanderbilt team makes important contributions
• ensure that all team members understand overall team goals and their roles
• answer questions posed by patients, trainees or staff to ensure understanding and
facilitate learning
I have a sense of ownership:
• take any concern (real, perceived, big, or small) seriously and seek resolution or
understanding - ask for help if the concern is beyond ability or scope of authority
• approach those who appear to need help or be lost and assist/direct them
appropriately
• clean up litter, debris and spills promptly or notify the best resource to keep the
medical center environment clean and safe
• remain conscious of the enormous cost of health care, teaching and research and
optimize resources while delivering exemplary service
I conduct myself professionally:
• recognize the increasing diversity of our community and broaden my knowledge of the
cultures of the individuals we serve
• adhere to department and medical center policies such as smoking, attendance and
dress code
• refrain from loud talk and excessive noises - a quiet environment is important to heal,

Transformational Leadership
Strategic Planning (1)
7
learn and work
• discuss internal issues only with those who need to know and refrain from criticizing
Vanderbilt in the workplace and in the community
• continue to learn and seek new knowledge to enhance my skills and ability to serve
• strive to maintain personal well-being and balance of work and personal life
I respect privacy and confidentiality:
• only engage in conversations regarding patients according to Vanderbilt policies and
regulatory requirements
• discuss confidential matters in a private area
• keep written/electronic information out of the view of others
• knock prior to entering a patient’s room, identify myself, and ask permission to enter
• utilize doors/curtains/blankets as appropriate to ensure privacy and explain to the
patient why I am doing this, ask permission prior to removing garments or blankets
I communicate effectively:
• introduce myself to patients/families/visitors, colleagues
• wear my ID badge where it can be easily seen
• smile, make eye contact, greet others, and speak in ways that are easily understood
and show concern and interest; actively listen
• recognize that body language and tone of voice are important parts of communication
• listen and respond to dissatisfied patients, families, visitors and/or colleagues
• remain calm when confronted with or responding to pressure situations
I am committed to my colleagues:
• treat colleagues with dignity, respect and compassion; value and respect differences in
background, experience, culture, religion, and ethnicity
• contribute to my work group in positive ways and continuously support the efforts of
others
• view all colleagues as equally important members of the Vanderbilt team, regardless
of job, role or title
• promote interdepartmental cooperation
• recognize and encourage positive behaviors
• provide private constructive feedback for inappropriate behaviors
Alignment of Strategic Planning
The strategic planning process for nursing is described in TL 3. This section responds to
the question of how the nursing strategic plan reflects the organization’s current and
Transformational Leadership
Strategic Planning (1)
8
anticipated strategic priorities. The most recent nursing strategic planning process was
completed in May of 2010. The organizational pillar goals, the Vanderbilt Medical Group’s
strategic plan and the known information related to healthcare reform provided the context
and foundation for the nursing strategic plan. On completion of the draft nursing strategic plan,
Marilyn Dubree, the Executive Chief Nursing Officer met with the CEO’s of the Vanderbilt
Medical Group, Vanderbilt University Hospital, Monroe Carell Junior Children’s Hospital, the
Vice Chancellor of Health Affairs and the Dean of the Vanderbilt School of Nursing to ensure
they perceived the nursing strategic plan aligned with those entities plans and that the strategic
plan was relevant to the future of the Medical Center.
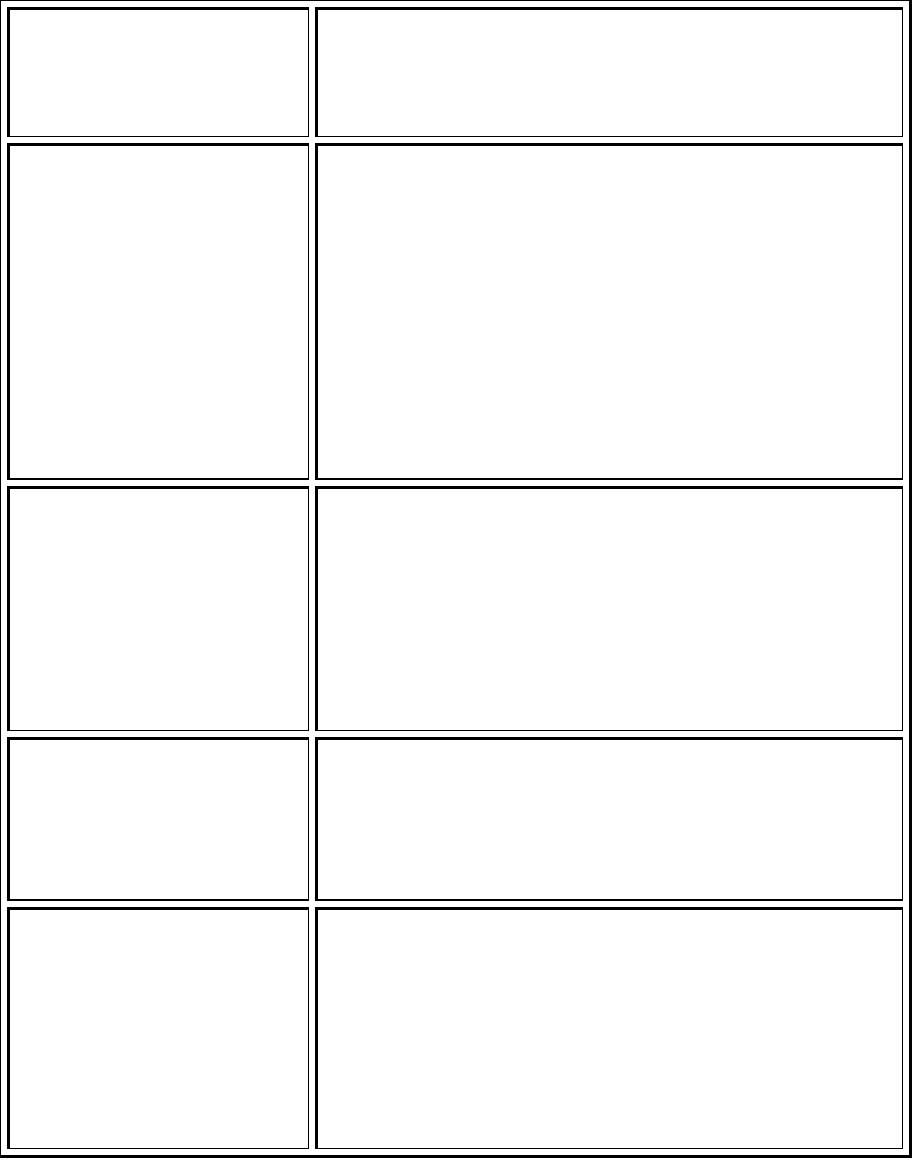
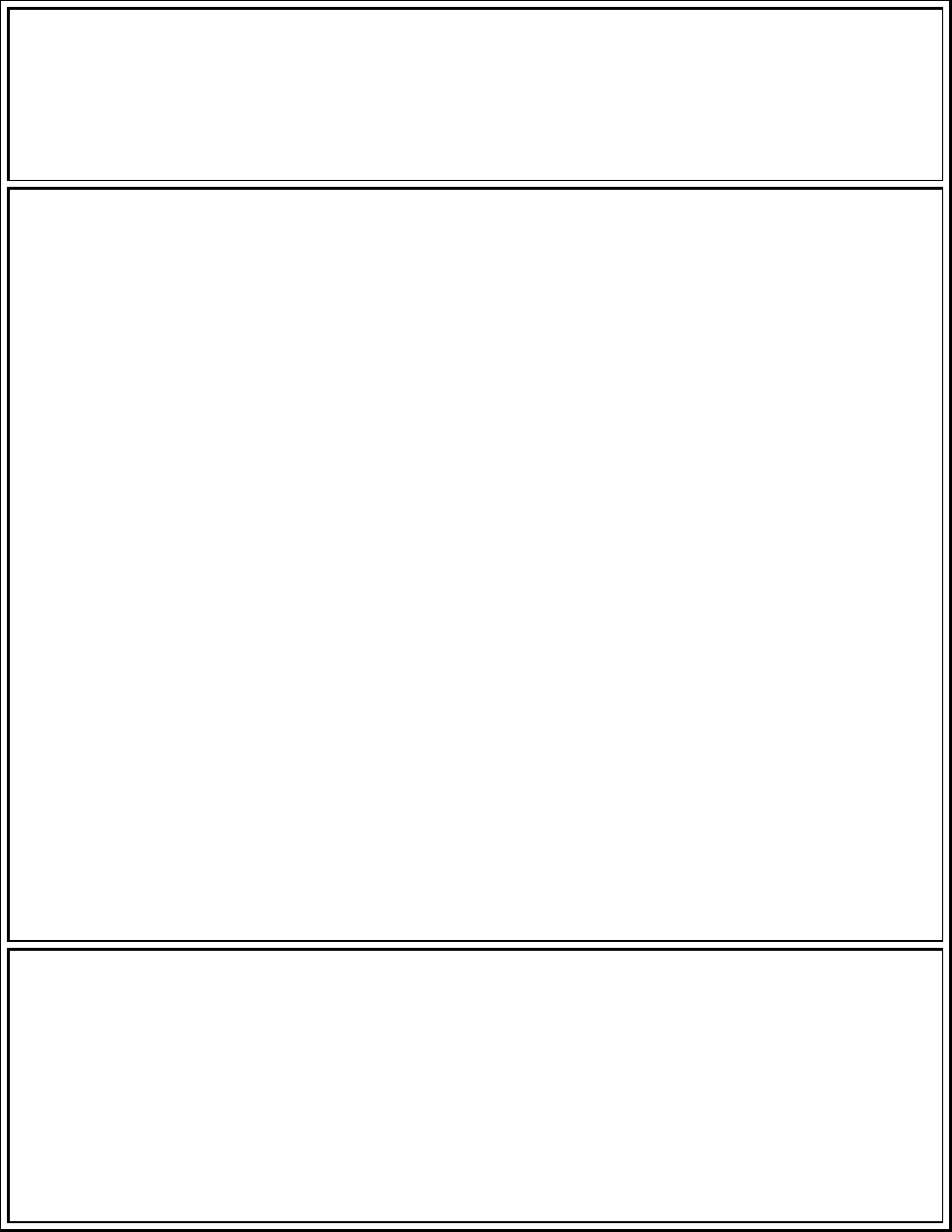
Several tables are presented that demonstrate alignment of the Vanderbilt Nursing
Strategic plan with the organization. Table TL 1-5 demonstrates the alignment of Vanderbilt
Medical Group Strategies and Nursing Strategies. (Nursing Strategic Plan in OO 3)
Table TL 1 -5: Alignment of Goals and Strategic Plans Fiscal Year 2010
VMG Strategies Nursing Strategies
Continuously improve patient outcomes using
evidence-based medicine: and innovative,
reliable, coordinated care practices.
Lead the nation in producing evidence that
will drive nursing practice, recognizing and
legitimizing the evolution of knowledge in a
rapidly changing environment. Create passion
and discipline for the translation of evidence
into practice that will optimize patient
outcomes.
Promote wellness and disease-prevention in
our communities.
Provide an exceptional personalized patient
experience through family-centered care and
value creation.
Transform the way in which health care is
delivered across the continuum in order to
ensure highly reliable personalized care, taking
advantage of the capabilities and unique
contributions of the entire care delivery team.
Be the healthcare employer of choice. Create a leadership model that will provide
current and future leaders the environments,
tools, evidence and skill development to be
innovative and transformational during a time
Transformational Leadership
Strategic Planning (1)
9
of health care reform and transition.
The Strategic Plan for Nursing outlines goals that support each strategy. Strategies and
supporting goals are outlined in Table TL 1-6. The crosswalk of the alignment of these goals
with the VMG strategic goals is presented in Table TL 1-7.
Table TL 1 – 6: Nursing Strategies and Goals
Nursing Strategies and Goals
I. Vanderbilt Personalized Patient Care Model
1 Statement of Strategy: Transform the way in which health care is delivered across the
continuum in order to ensure highly reliable personalized care, taking advantage of the
capabilities and unique contributions of the entire care delivery team.
GOALS
1.1 Determine what brings value to patients, makes a difference and creates breakthroughs
1.2 Understand the impact of who brings the right skill set and resources to achieve a
personalized healthcare model
1.3 Understand and design systems to maximize the benefit and utilize the full talents of the
healthcare team
II. Evidenced Based Practice and Effective Processes
2 Statement of Strategy: Lead the nation in producing evidence that will drive nursing
practice, recognizing and legitimizing the evolution of knowledge in a rapidly changing
environment. Create passion and discipline for the translation of evidence into practice
that will optimize patient outcomes.
GOALS
2.1 Establish/create nursing infrastructure dedicated to driving the cycle of EBP
2.2 Develop and implement core training systems for evidenced based practice processes
targeted to role requirements
2.3 Ensure the alignment of evidenced based practice with internal and external benchmarking
and quality improvement priorities
Transformational Leadership
Strategic Planning (1)
10
2.4 Complete gap analysis for evidenced based practice and create a work plan for moving
forward
2.5 Disseminate and publish; broadcast to mark what is being accomplished in evidenced based
practice
III. Transformational Leadership and Professional Development
3 Statement of Strategy: Create a leadership model that will provide current and future
leaders the environments, tools, evidence and skill development to be innovative and
transformational during a time of health care reform and transition.
GOALS
3.1 Develop transformational leaders who can create and transform
programs/products/environments to meet the patient population needs and VUMC
organizational goals (People, Quality, Safety, Finances, Growth, and Innovation).
3.2 Develop a recruitment and retention philosophy that supports flexible standard and
consistent requirements for leadership practice.
3.3 Provide organizational learning opportunities for the individual leaders and leadership
teams to learn together and obtain or create tools to meet their desired objectives
3.4 Define the leadership model that is transformational and flexible with leadership
competencies and a menu of tools
Table TL 1 - 7: Cross walk of alignment of VMG strategic goals and Nursing Strategic Goals
Vanderbilt Medical Group Strategic Goals Nursing Strategic Goals
Clinical Growth & Capacity
Establish clinical service capacity,
infrastructure, and desired growth in support
of VUMC goals.
Operational Efficiency
Achieve optimal service and care coordination
by improving the operational efficiency and
effectiveness of the Vanderbilt clinics through
1.2 Understand the impact of who brings the
right skill set and resources to achieve a
personalized healthcare model
1.3 Understand and design systems to
Transformational Leadership
Strategic Planning (1)
11
the design and implementation of a consistent
and measureable operational platform that
meets patient/family expectations, simplifies
work processes for physicians and staff,
supports future growth, and creates an
environment of innovation.
maximize the benefit and utilize the full
talents of the healthcare team
2.4 Complete gap analysis for evidenced
based practice and create a work plan for
moving forward
Continuous Improvement of Outcomes
Demonstrate continuous improvement of
patient outcomes through the use of
evidence-based medicine and quality and
safety science best practice
2.3 Ensure the alignment of evidenced based
practice with internal and external
benchmarking and quality improvement
priorities
Development & Training
Improve team effectiveness, care, and service
outcomes in patient care through
organizational development and training
programs targeted to leadership
development, support staff education, clinical
team training, and orientation.
2.2 Develop and implement core training
systems for evidenced based practice
processes targeted to role requirements
3.1 Develop transformational leaders who can
create and transform
programs/products/environments to meet the
patient population needs and VUMC
organizational goals (People, Quality, Safety,
Finances, Growth, and Innovation).
3.3 Provide organizational learning
opportunities for the individual leaders and
leadership teams to learn together and obtain
or create tools to meet their desired
objectives
Maximize Value
Maximize the value of VMG to the
organization (internally), locally, and
nationally.
1.1 Determine what brings value to patients,
makes a difference and creates
breakthroughs
2.5 Disseminate and publish; broadcast to
mark what is being accomplished in evidenced
based practice
Management & Governance
Align management and governance of the
2.1 Establish/create nursing infrastructure
dedicated to driving the cycle of EBP
Transformational Leadership
Strategic Planning (1)
12
VMG/TVC for execution of the strategic plan
and the meet the interests of the VUMC in the
transformation of practice.
3.2 Develop a recruitment and retention
philosophy that supports flexible standard and
consistent requirements for leadership
practice.
3.4 Define the leadership model that is
transformational and flexible with leadership
competencies and a menu of tools
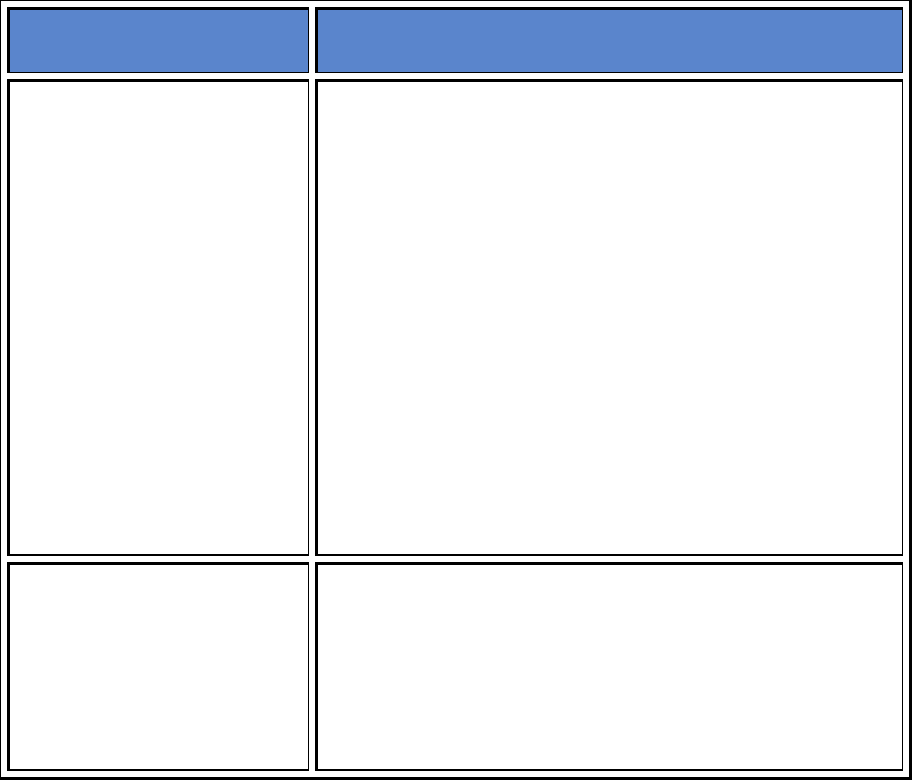
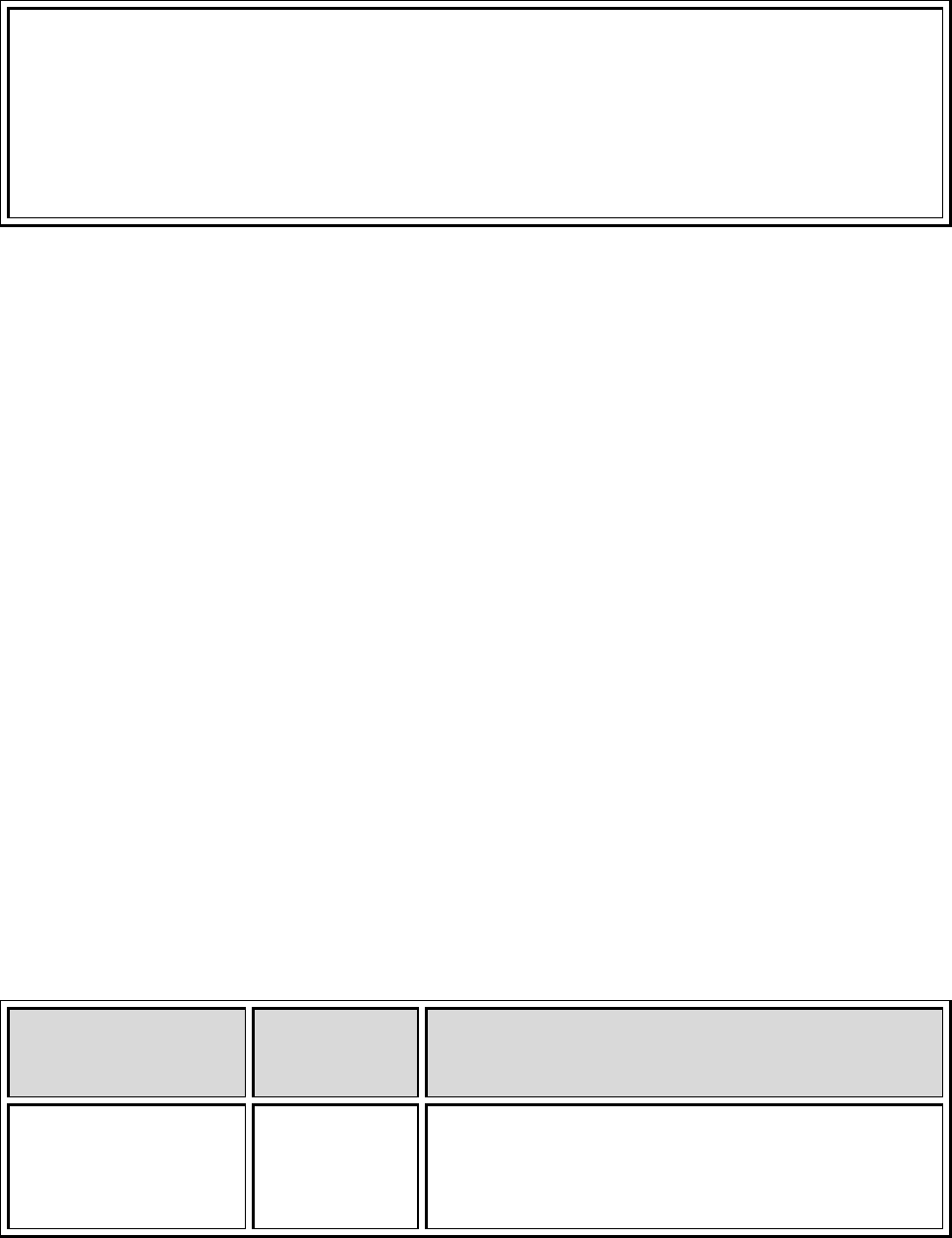
We have adopted an approach to operations based on the five pillars of people, service,
quality, finance and innovation. Annually, the organization develops pillar goals to guide
operational focus for the coming year. A Blueprint for Quality that has been collaboratively
developed for the entire organization and the Nursing Quality Performance Plan guide the
creation of the annual quality pillar goals which are represented in Table TL 1-8. Both of these
documents are available in Organizational Overview – Question 3. Table TL1-8 represents our
approach to annual 5 pillar goal establishment and the crosswalk of organizational pillar goals
and nursing pillar goals.
Table TL 1 – 8: Crosswalk of organizational pillar goal targets with nursing pillar goals
2011 Organizational Pillar Goals 2011 Nursing Pillar Goals
People
Retention at 18 months after hire – 67.5%
Overall turnover (all employees) – 11.5%
People
Retention at 18 months after hire – 67.5%
Overall turnover (all employees) – 11.5%
Nursing Turnover – 11.8%
Service Pillar (Patient Satisfaction)
Overall Quality of Care – perform at 95
percentile
Overall Teamwork between doctors,
providers, nurses and staff – perform at 95
percentile
Patient engagement – perform at 95
percentile
Improve VMG access to level of 60% of
Service Pillar (Patient Satisfaction)
Overall Quality of Care – perform at 95
percentile
Overall Teamwork between doctors,
providers, nurses and staff – perform at 95
percentile
Patient engagement – perform at 95
percentile
Improve VMG access to level of 60% of
Transformational Leadership
Strategic Planning (1)
13
new patients being seen within 15 days of
requesting appointment
new patients being seen within 15 days of
requesting appointment
Quality
Observed to expected mortality at 0.70
15% reduction in healthcare acquired
infections (SIR score of 1.11) as
measured by the sum of Central line
acquired blood steam infections,
ventilator acquired pneumonia,
catheter associated urinary tract
infections
15% reduction in preventable
healthcare adverse events as
measured by the sum of falls, pressure
ulcers, medication errors.
Improve intra-professional
communications within and across all
care settings during transfer ad
transitions of care and during
procedures
Design and establish a coherent quality
improvement learning system with
defined tools and methods to foster
continuous learning for continuous
improvement
Achieve top performance in clinical
programs
o Stroke – 91%
o Pneumonia – 90%
o Heart failure – 95%
o SCIP – 94%
o OPPS – 94%
o Acute MI – monitor
o Diabetes – to be developed
o Pediatric asthma – TBD
Quality
Observed to expected mortality at 0.70
Healthcare Acquired Infections
Central line acquired blood steam
infections SIR score of 1.31
Ventilator acquired pneumonia SIR
score of 1.24
Catheter associated urinary tract
infection SIR score of 0.63
Surgical site infection SIR score of 1.09
Hand hygiene – 90%compliance
Preventable healthcare adverse events
Pressure ulcers per 1000 patient days –
0.86
Falls per 1000 patient days – 3.00
Medication errors per 1000 patient
days – 3.81.
Intra-professional communications
Design standardized process and tools
for handovers and spread to 3 areas
Design and establish a coherent quality
improvement learning system with defined
tools and methods to foster continuous
learning for continuous improvement
Develop prototype of standardization
process for admission and discharge
medication reconciliation
Achieve top performance in clinical programs
o Stroke – 91%
o Pneumonia – 90%
o Heart failure – 95%
o SCIP – 94%
o OPPS – 94%
o Acute MI – monitor
Transformational Leadership
Strategic Planning (1)
14
o Diabetes
–
to be developed
Pediatric asthma – TBD
Finance and Growth
Results of operations - $106.4 million
Discharges – 55,360
Ambulatory visits – 1,557,302
Surgical procedures – 47,472
Cost per discharge - $16,288
Cost per visit - $489
Finance and Growth
Results of operations - $106.4 million
Discharges – 55,360
Ambulatory visits – 1,557,302
Surgical procedures – 47,472
Cost per discharge - $16,288
Cost per visit - $489
Innovation
Warfarin– proof of concept
MyHealth@VU – results of proof of
concept
Achieve reduction in growth of Vanderbilt
Health Plan costs – results of proof of
concept
Diagnostic Management team – results of
proof of concept
Integration of pharmacogenomic
information into clinical decision support
infrastructures
Presentation of genomic data to
individuals
Innovation
Warfarin
Improve over baseline INR in-range by
20% (outpatient coumadin clinic)
MyHealth@VU
Improve to 65% the number of
patients with blood pressure in control
without adversely affecting satisfaction
scores (VMG nurse managed patients
through MyHealth@VU)
Transformational Leadership
Strategic Planning (2)
15
Strategic Planning
Source of Evidence 2
Describe and demonstrate how nurses at every level – CNO, nurse administrators, and direct-
care nurses – advocate for resources, including fiscal and technology resources, to support
unit/division goals.
There are a multitude of ways nurses at all levels influence access to resources to meet
unit and department goals. Starting at the staff level, all staff have direct access to nurse
managers as well as through Unit Board meetings, staff meetings, unit based quality and service
meetings. Managers practice leader rounding intentionally asking “Do you have the tools to do
your job” and “What resource or systems problems exist that are barriers to effective patient
care”. Leaders are expected to actively access required resources and/or to remove identified
barriers to support patient care. Staff nurses also sit on organization wide committees and
councils providing feedback to managers and administrators in nursing and from across the
Medical Center.
Managers meet with the administrator responsible for their area regularly both one and
one and with their peers. During these group meetings common resource issues are identified
and accountability for access resources defined. Inpatient managers have access to the Medical
Economics Outcomes Committee where supply purchases are considered. This committee
organizes trials for new supplies and supply replacement and equipment.
Nursing administrators and executives are actively involved in creating and prioritizing
the capital list for all entities each year. Nursing leaders are responsible for demonstrating need
and return on investment for new items that are not replacement items. Managers and
administrators work closely with Clinical Engineering leadership to be certain critical equipment
is replaced according to the life cycle and maintenance and repair requirements of the
equipment is followed. [TL2-Exhibit A-1–VUH capital list with leaders] Nursing administrators
play a pivotal role in establishing IT priorities. Nurses at all levels participate in design shops and
regular meetings to advocate and influence nursing IT development and purchasing plans that
support the role of the professional nurse and optimize patient outcomes.
Transformational Leadership
Strategic Planning (2)
16
Examples
IT Design Shops
Information technology annual planning process – Although there has been a long
history of end users being involved in the IT decision making, there had not been a structured
process for nursing input. This sometimes resulted in the lack of alignment between IT priorities
and outputs and organizational goals. The current process has been perfected over the last 5
years. It has put the operational planning process team members with a strong nursing voice in
the driver seat for IT prioritization. The process results in a shared vision, clear priorities and
measurable outcomes. The process also includes quarterly check in as objectives and priorities
change over the year.
The prioritization occurs in “Design Shops” which are held in the Center for Better
Health. These design shops depend on large groups of multiple levels of employees coming
together. The participants work in small groups reporting out progress to the larger group. The
recommendations and decisions in the day(s) of Design Shops are iterative and continually
draw on the experts in the field to inform IT of needs, desired outcomes and priorities. The final
output of the Design Shops is a “Swim Lane” document that creates timelines and deliverables
for each project. The document is used by users to evaluate the progress of the IT teams. [TL2-
Exhibit B-1-2010 Design Shop –Patient Engagement, TL2-Exhibit B-2-Heart Failure Teaching
Record]
In one of the early design shops several nursing related IT projects were identified.
The need was identified to standardize admission and shift skin assessments to be
consistent with national guidelines. As a result of this, changes were made to the
electronic order entry system and the nursing documentation system. The changes were
piloted for staff feedback and then rolled out across the enterprise in the spring and
summer of 2009.
Ventilator acquired pneumonia (VAP) and compliance with the VAP bundle were
problematic in the nursing ICU’s. The participants in the design shop recognized the
opportunity for IT to provide reminders and feedback loops for nurses to improve
compliance with the bundles. As a result of the design shop both the electronic order
entry system and the nursing documentation system were improved.
In addition, nurses were provided with a dashboard that is constantly open on clinical
work stations for the patients on the unit. Each part of the bundle has a red, yellow and green
Transformational Leadership
Strategic Planning (2)
17
indicator flag for each patient. Red means the task in the bundle is not complete and overdue
for a particular on a patient. Yellow means that it is nearing time for a particular task to be
completed. If the steps in the bundle are complete, the task box is green. Through the use of
the VAP dashboard as a reminder and flag to nurses regarding what is due, over- due and
complete on their patients, the VAP standardized infection ratios (SIR) fell from 2.59 in MCJH in
February of 2008 to a SIR of 0.7 in July of 2010 and in the adult hospital the Sir went from 2.23
to 1.75 in the same time frames referenced.
Nurses identified at the design shop that the electronic medical record made it difficult
to see all of the information necessary to care for the patients efficiently. Nurses stated
they could not easily read the patient story and understand what had happened, was
happening and was going to happen to a patient. As a result of this identification, the
Overview of Patient Care (OPC) was developed which aggregates all necessary
information for the nurse in one location.
Although the pilot was well received, changes were made to “de-clutter” the overview
to make it easier to read. In addition, a charge nurse snapshot was developed to include all of
the information charge nurses need to make appropriate assignments on patients. The
overview of patient care has had broad adoption across the inpatient organization and has
been adopted as a useful tool for physicians as well as nurses.
Based on feedback at a design shop that nurses needed more alerts and reminders, a
screen saver was developed for all clinical work stations which displays visual reminders
and alerts for nursing staff when there are new orders for a patient, new lab results or
interventions are necessary.
Accessibility to Human Resources at Off-Campus Site
Opening of the 100 Oaks outpatient campus provided many challenges for Janice Smith,
RN, MS, the Chief Administrative Officer and the Nursing leader at 100 Oaks. She became aware
that the human resource needs of the 1,000 employees at that campus would be difficult to
manage with Human Resource (HR) functions only available approximately 6 miles away. Both
managers and employees have many human resource department needs including recruitment,
position changes, hiring, termination, and employee relations issues. These functions have
traditionally been spread across many departments in HR. Janice set a goal to provide as much
on site HR consultation as possible. Janice worked with Veronica Burns, the Director of Human
Resources to develop a new title of HR generalist. This HR employee would be able to manage a
wide variety of issues as opposed to the traditionally highly specialized staff in Vanderbilt’s HR
Transformational Leadership
Strategic Planning (2)
18
Department. Janice successfully worked with David Posch, the CEO of the VMG and the
Vanderbilt Clinics to secure funding for the position. The position was funded through VMG but
dually reports to Janice and HR leadership. The position was filled and HR service began in
October of 2009. [TL2-Exhibit C-1-HR Generalist Job Description]
Resources to Change Practice
Kathy Burns, MSN, RN, a clinical nurse specialist in the CVICU became aware of research
related to improved neurological survival for out of hospital arrest patients when their body
temperature is cooled for 24 hours. Kathy partnered with the Medical Director of the CVICU,
John McPherson and developed a program proposal for this effort. She worked through the
Medical Economics and Outcomes Committee to complete trials of the necessary cooling
equipment.
Kathy discovered interest for this technology across other ICU’s. She began to work
through the Institutional Critical Care Committee to develop the necessary justification for the
devices. She worked with purchasing and with the vendor of the selected device to develop a
quote for the technology. Through the capital prioritization process in the Vanderbilt Heart and
Vascular Institute, funds were secured for this device.
To date, 38 of the 79 patients or 48.1% who were “out of hospital arrests” survived and
are neurologically intact. This is compared to a historical 25-30% survival rate in un-cooled
cardiac arrest victims admitted alive to hospital, with a lower rate of good neurologic outcome
despite survival. [TL2-Exhibit D-1-Cooling Release, TL2-Exhibit D-2-Hypothermia]
IT Leadership for Nursing
VUMC has been listed as one of the “most wired” hospitals and health system in the
country. There is a large informatics team that develops and implements healthcare
technologies that enhance the delivery of patient care. Our Executive CNO, Marilyn Dubree
MSN, RN, NE- BC, recognized the need for a nursing leader in informatics applications within
the healthcare system. She observed that technology was beginning to define nursing practice
and noted it would either enhance or detract from the professional role of the nurse depending
on the implementation and use. Marilyn recognized that the science of the application of
technology to nursing practice in a healthcare system required a knowledgeable and dedicated
resource.
Marilyn created a position to oversee clinical applications of technology and enhance
the practice of nursing. The position created the nursing informatics bridge between the
Transformational Leadership
Strategic Planning (2)
19
hospital and the clinics. The person selected for this position would articulate a strategy to
ensure that nursing needs were met in an ever increasing highly automated environment.
Deborah Ariosto, RN, MSN, PhD(c) (doctoral candidate in Nursing) joined Vanderbilt as the
Director of Patient Care Informatics on November 5, 2008. Since her arrival, she has completed
the assessment of nursing informatics systems and processes and begun to influence change in
the system.
Deborah has been very active. Since she began in her role she has worked with staff and
leaders to standardize and simplify pain documentation. She has developed a new method,
system and tool for documenting patient education for heart failure patients. She directs
changes to the nursing documentation system through simplification and standardization.
Deborah as created the QERI-Ops group which is charged with quality, education, research and
informatics initiatives with the strategic planning and operational structures of Vanderbilt
nursing.
Capital Budget
As part of the budget process annually, all of the entities submit the prioritized list of
the capital needs in their area. These are generally submitted in the major Capital Category
(>$100,000), routine capital (<$100,000 but >$50,000) and discretionary (<$50,000). The
Vanderbilt Heart and Vascular Institute spans the continuum of care and includes operations
and nursing in the following areas:
5 Inpatient units
1 on campus clinic for cardiology, vascular and cardiac surgery (50,000 visits)
14 off campus clinics (20,000 visits)
Non-invasive diagnostic testing s on campus and off including nuclear cardiology,
Cardiac MRI, Echosonography, stress testing, autonomic function testing, vascular
testing
Cardiac Catheterization labs
Electrophysiology labs
Transformational Leadership
Strategic Planning (2)
20
VHVI does not have a capital allocation. Capital must be submitted to both the VMG and
VUH because VHVI operations sit both in VUH and the VMG and both of these entities have
their own capital allocations.
The diversity of services provided in the Heart Institute makes capital submission to two
different entities challenging every year. Robin Steaban RN, MSN is responsible for operations
and nursing in VHVI and is responsible for capital submission. She has created an Operations
Council within VHVI. The Council is the operating decision making body of VHVI for all things
that are within the budget and the recommending body for all things outside of the budget. All
of the Medical Directors, their associated nursing manager partners and VHVI administrators
are voting members of the Council. Robin works through this structure to have physician and
nursing leaders prioritize the capital list for VHVI based on programmatic priorities and clinical
need. Nursing leaders and physicians have equal voice in the process. [TL2-Exhibit-E-1-
Operations Council Minutes]
Robin then takes the capital needs to both the VMG and VUH and works with the
administrative teams at that level to prioritize VHVI needs against others in the organization.
Robin is able to work with all administrators to agree what capital should be purchased with
consideration of the entire organization in mind. She is present for the capital negotiations and
is able to advocate for the needs within VHVI based on return on investment, patient safety and
quality risk, potential impact to the business for unplanned failure. This participation in the
organization wide process allows Robin to communicate with VHVI Medical Directors, Nursing
Managers and Administrators why capital decision were made. The process builds trust in the
organization and keeps staff and faculty connected to organizational priorities outside of VHVI.
[TL2-Exhibit-E-2-Five year Capital Plan]
“Vanderbilt Shockers”
Dawn Sabine, RN, BSN is a nurse in the Vanderbilt Heart and Vascular Institute. She
works as a specialty nurse with arrhythmia patients. There is a significant population of patients
with CIEDs (cardiac implantable electronic devices). Dawn is the expert in caring for these
patients. She recognized that although this therapy is life saving, it is also a life altering
experience. Patients must make modifications to their lives once they have had a CIED placed.
She recognized CIED patients needed additional support. Dawn researched what other
institutions were doing and developed a proposal for a CIED support group for patients and
families. She advocated with leadership in VHVI for the funding and clerical support to manage
Transformational Leadership
Strategic Planning (2)
21
these support groups. In 2007, the support for the group was successfully budgeted and Dawn
held the first meeting of the “Vanderbilt Shockers”.
The group typically has 80-100 people in attendance. She has worked on behalf of the
patients to advocate for resources for the meetings that takes place 3-4 times per year. These
resources include speakers, space, recruiting volunteers as well as monetary resources.
The group has remained active and has been positively reviewed in a patient feedback
tools. By increasing patient education and allowing for greater access to health care providers,
patients have an opportunity to learn from experts as well as other patients about how to
adjust their lives to accommodate and thrive with an ICD.
Dawn has just started an advisory board that meets on a periodic basis on behalf of the
other ICD patients. The advisory board makes suggestions as to future topics, speakers and if
needed, will contact new patients who are having trouble or would like to speak with another
patient with an ICD. [TL2-Exhibit F-1-Invitation]
Can I help you find your way?
Tom Conner, RN, Manager of the Medical Center East PACU reported that staff noted
many lost visitors and families outside of the PACU wandering the halls. At times, they have
inadvertently entered the operating rooms. Staff consistently offers to assist people who
appear lost. Numerous times when a patient is in route to the OR the gurney is stopped so the
Anesthesia personnel can provide directions. Guest Services did not seem to be an option for
the 3
rd
floor. In lieu of Guest Services, Tim contacted Julie Bulger in volunteer services. In
cooperation with Beth Pittman of Guest Services, there will soon be a volunteer on the 3
rd
floor
scouting lost people in 2 hour time blocks.
Transformational Leadership
Strategic Planning (3)
22
Strategic Planning
Source of Evidence 3
Describe and demonstrate the strategic planning structure(s) and process(es) used by nursing
to improve the healthcare system’s: 1) effectiveness and 2) efficiency.
Our strategic planning efforts are multi-tiered and multi-focused. The foundation for all
planning efforts is the VUMC organizational plan. The plan is created annually at the most
senior executive levels of the organization and sets the direction of VUMC. There are entity and
Institute strategic planning efforts that produce plans consistent with the overall VUMC
strategic planning but specific to the entity or Institute. In addition, there is a specific strategic
planning process for nursing within the organization that is lead by Marilyn Dubree, MSN, RN,
NE-BC, Executive Chief Nursing Officer.
Each of these plans cascade off of the VUMC. In addition, each of these plans is heavily
influenced if not lead by nursing leaders. Nurses across the organization contribute and
influence the strategic plans of the organization, entities and Institutes. The following will
describe efforts related to VUMC, Vanderbilt entity and institute strategic planning efforts and
the structures and processes that provide nurses at every level an opportunity to influence
these plans to improve the effectiveness and efficiency of the healthcare system.
Vanderbilt Nursing Strategic Planning Structure and Process
In 2008 many changes were occurring in our nursing leadership. The organization had
grown to the extent that a more robust nursing leadership structure was required. In that year
Marilyn added several positions that reported to her as she moved into the Executive Chief
Nursing Officer role. Those positions included a CNO for VUH and for the Vanderbilt Medical
Group in addition to the existing CNO of Monroe Carell Junior Children’s Hospital. In October of
2008, Marilyn Dubree, the Executive Chief Nursing Officer (ECNO) convened all nursing
administrators for a several day retreat. The goal of that retreat was to solidify the leadership
infrastructure for nursing as well as the charters for the nursing leadership structures. Another
deliverable of the retreat was a draft mission and vision statements for nursing.
Marilyn gave all nursing administrative leaders (the Nursing Administrative Board i.e.,
NAB) an opportunity to review the organizational documents related to the mission and vision
of the organization. She then asked all to participate in a dialogue about the content of these
Transformational Leadership
Strategic Planning (3)
23
documents and how they should inform the development of a nursing vision and mission. After
much discussion, a list of agreed upon thoughts was created.
The Nursing Executive Board (NEB) members then left the NAB retreat armed with what
they had heard from all nursing administrators. They began the work of crafting the mission
and vision statements for nursing. Each member of NEB worked privately and then joined with
the entire NEB group to share their ideas and collaborate on the final draft of a mission and
vision statement. After 2 hours, the draft was presented to the larger NAB. The document was
fully endorsed and has become the Vision and Mission of nursing at Vanderbilt University
Medical Center.
Several more workshops and retreats focusing on the development of the nursing
strategic plan were held in the months that followed. Consistent with the roles of Boards in the
Nursing Bylaws, Marilyn worked closely with the members of the strategically focused Nursing
Executive Board (NEB) through the strategic planning process. In April of 2009, the NEB worked
with Marilyn to identify three strategic priorities based on a review of internal and external
priorities for nursing.
Through June and July of 2009, Marilyn reviewed the three strategic priorities with the
Vice Chancellor, the Deputy Vice Chancellor and CEO of Vanderbilt Hospitals and Clinics and the
CEO’s of the VMG and Clinic, the Children’s Hospital and Vanderbilt University Hospital. In
addition, Marilyn reviewed the three strategies with managers of the Medical Center and at the
Staff Nurse Councils. Feeling confident about the direction of the strategic plan, Marilyn
convened an NEB retreat in the November of 2009 to begin to plan the tactics to attain the
strategic priorities.
Throughout 2010, the Be the Best teams have begun to focus on the beginning
implementation of the nursing strategic initiatives.
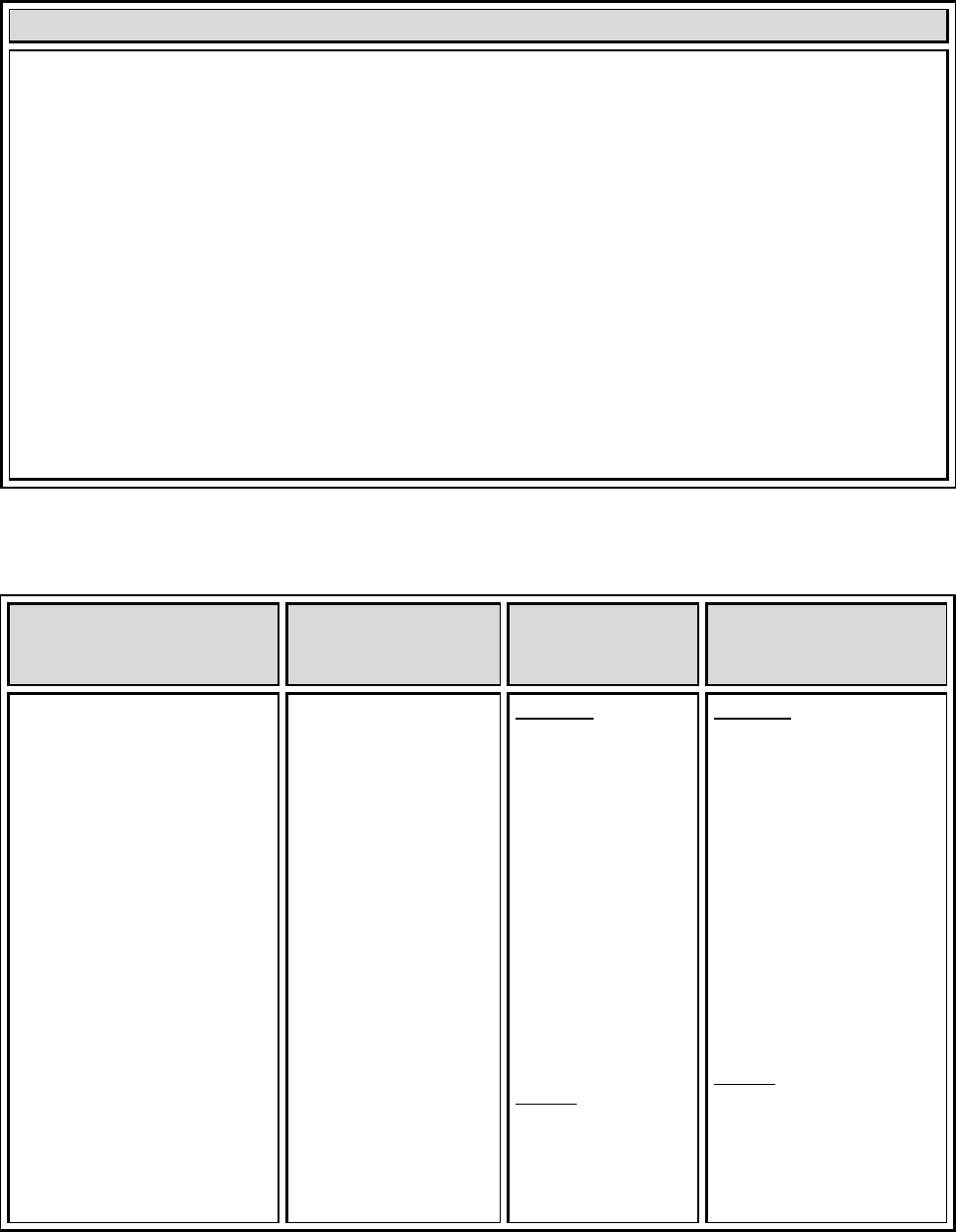
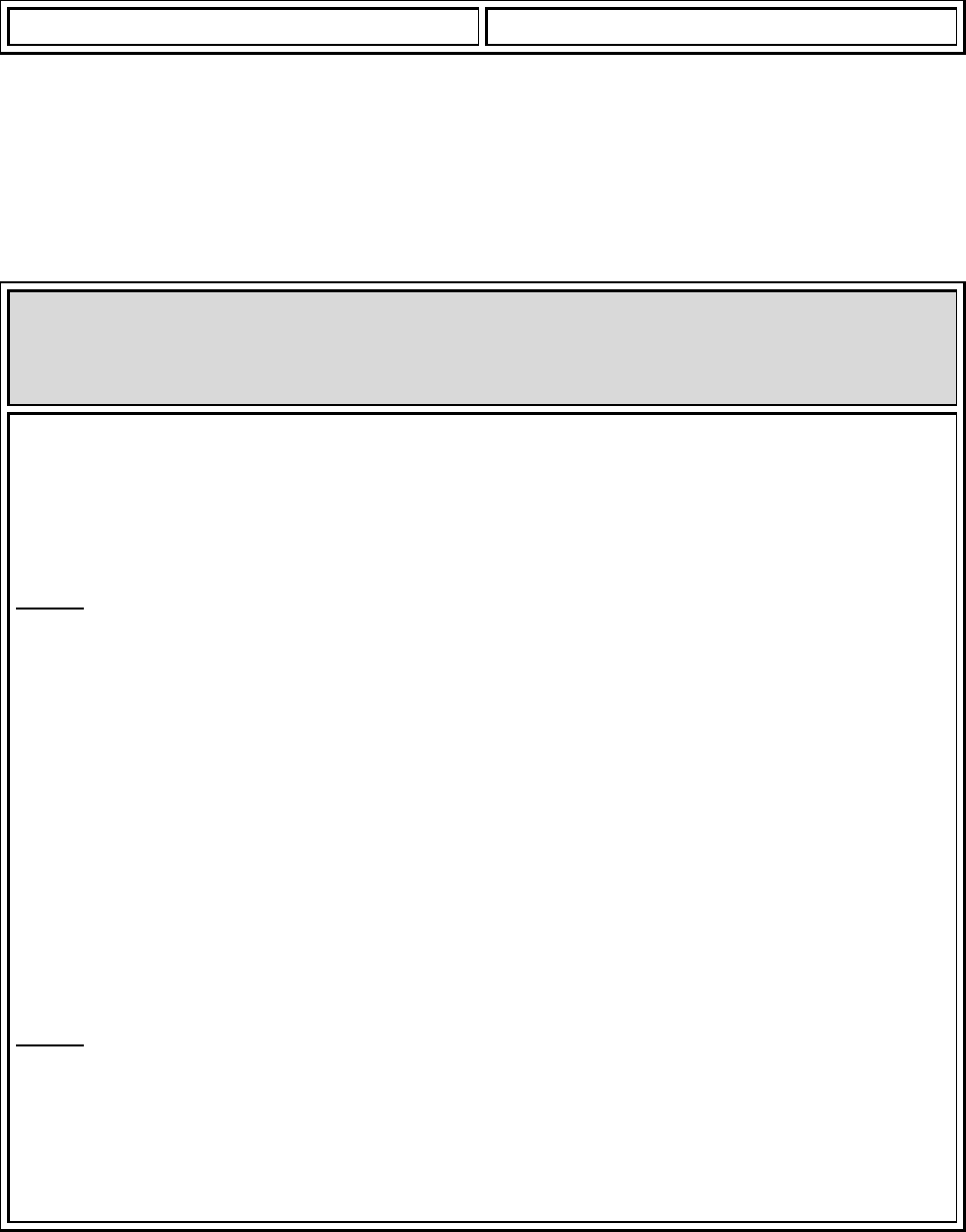
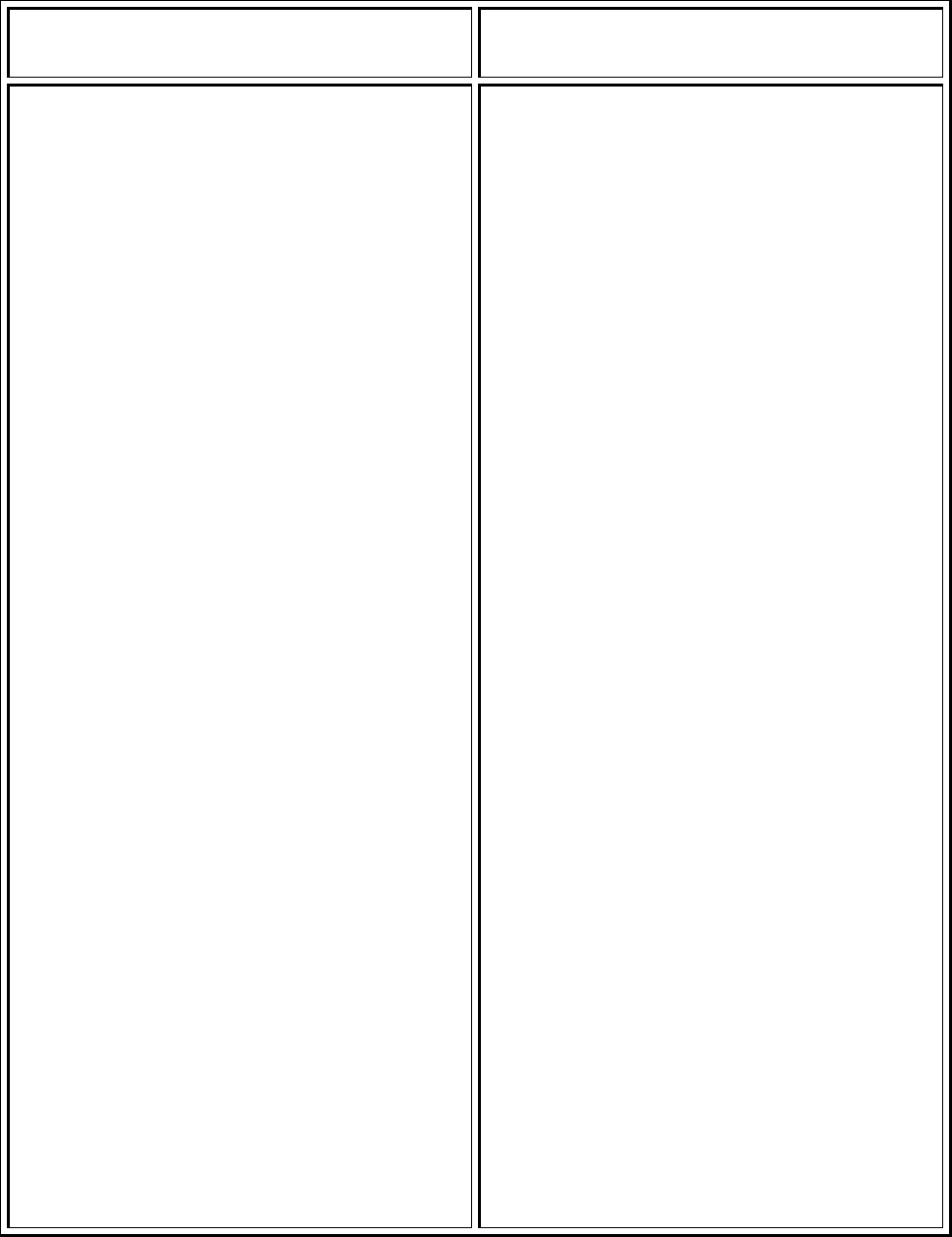
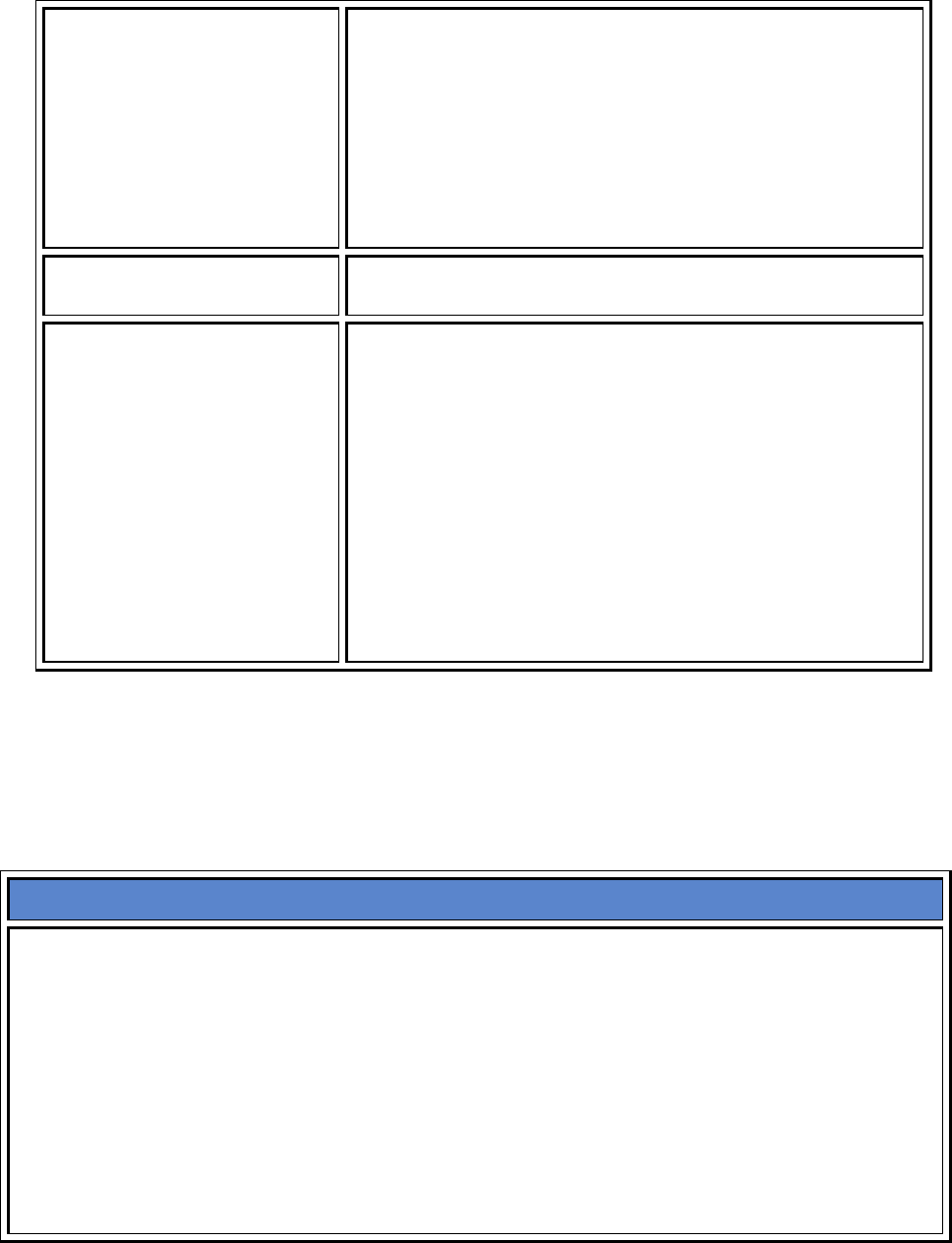
The Development and review process of the strategic plan is shown in Chart TL 3 – 1.
Chart TL 3 - 1: Process for Development of Current Nursing Strategic Plan
Structure: NAB Function: Inform
development of Mission and
Vision
Structure: NEB
Function: Draft Mission and
Vision for Nursing
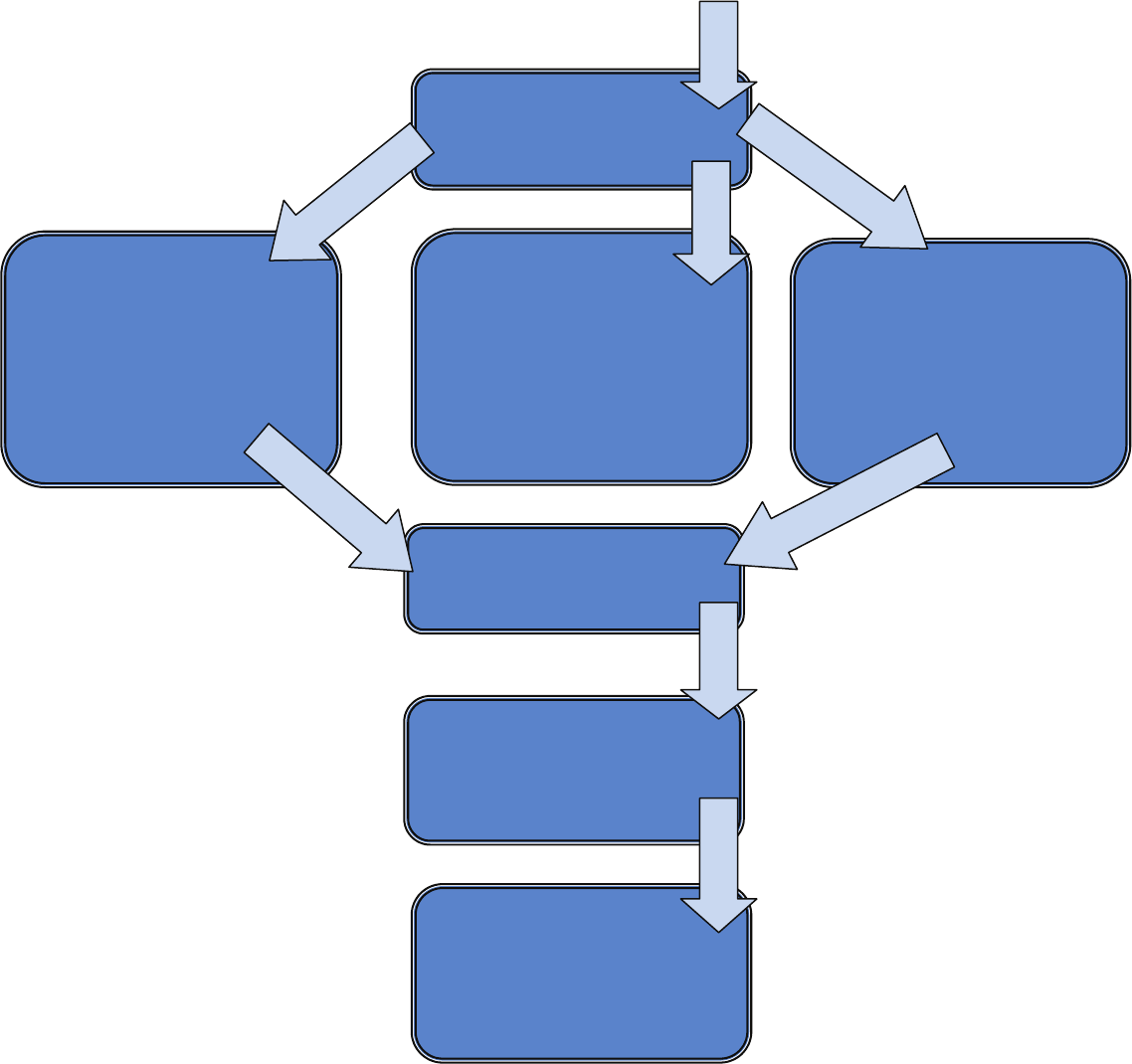
Transformational Leadership
Strategic Planning (3)
24
Vanderbilt University Medical Center Planning
Structure: VUMC Nursing
Managers
Functions: Endorse /
recommend changes to
Nursing Strategic Plan
Statements
Structure: Vice Chancellor,
Deputy Vice Chancellor, Entity
CEO’s
Functions: Endorse /
recommend changes to the
Nursing Strategic Plan
Statements
Structure: Staff Nurse Councils
Functions: Endorse /
recommend changes to the
Nursing Strategic Plan
Statements
Structure: NEB
Function: Draft Strategic Plan
Priority Statements
Structure: NEB
Function: Draft Strategic Plan
Tactics
Structure: Administrative Affairs
Function: Final Approval of
Strategic Plan
Structure: Be the Best Task
Forces
Function: Implement tactics to
achieve Nursing Strategic Plan
Transformational Leadership
Strategic Planning (3)
25
VUMC executives support an annual planning process that is build around the five pillars
of performance used by Vanderbilt to guide organizational direction and focus. The pillars and
the 2011 goals are represented in Table TL 3 – 1.
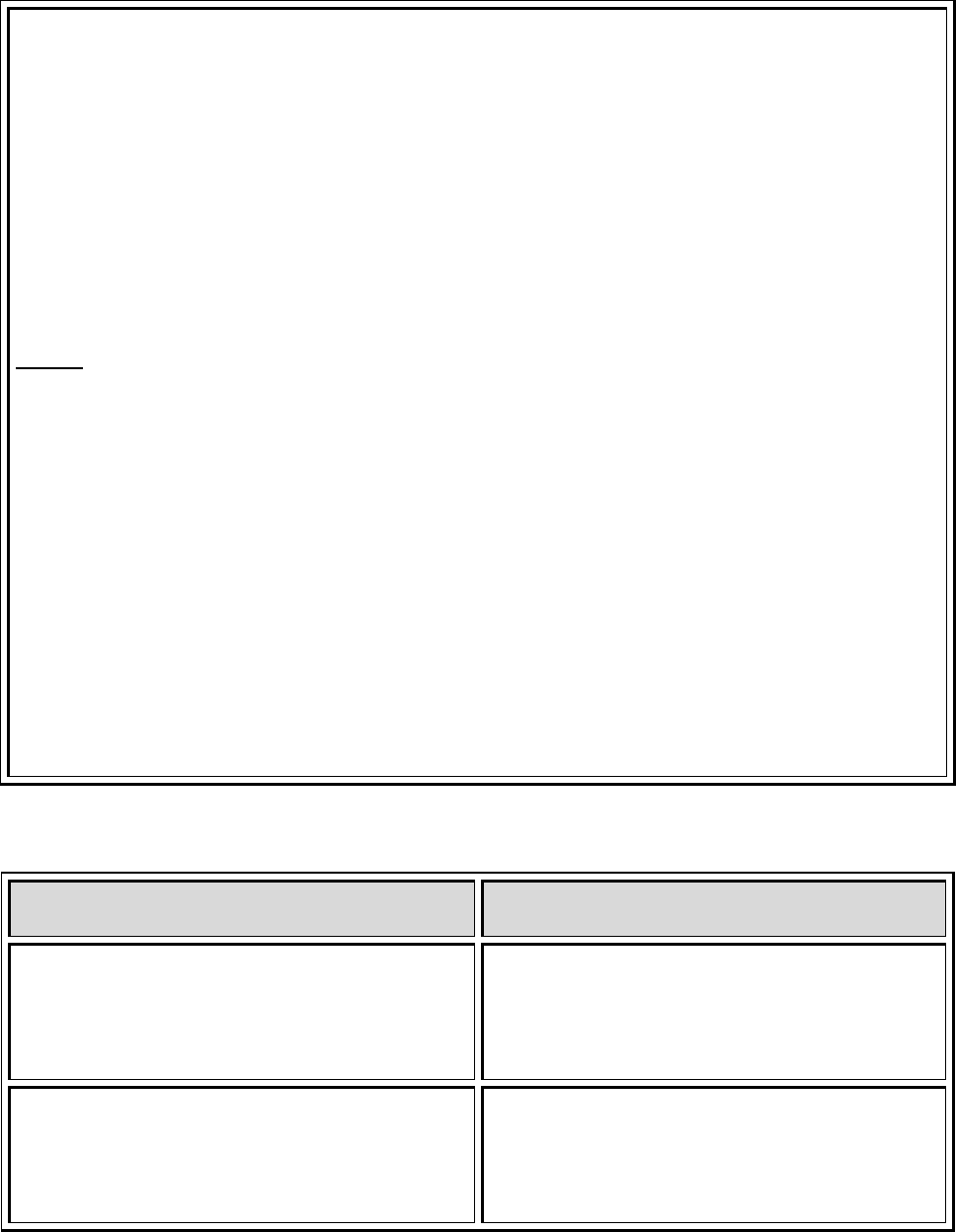
Table TL 3 - 1: Vanderbilt University Medical Center Pillar Goals
People
Service Quality
Growth and
Finance
Innovation
We nurture a
caring, culturally
sensitive, and
professional
atmosphere as
we
continuously
invest
in the individual
and
collective
aspirations
of our people
Collegiality is a
central
characteristic
of our culture
and
defines how we
serve our
patients,
those we teach,
and the local
and worldwide
community
We relentlessly
pursue and
measure
ourselves against
the highest
quality
performance in
all
areas, from
patient
care to
scholarship
We invest our
resources in a
manner that
supports
our long-term
obligation to
society;
to achieve local,
national and
worldwide
impact in
improving health
We seek
excellence
and leadership
as
we advance our
systems of care,
educational
practices and our
commitment to
discovery
2011 Goals:
New hire
retention
After 18 months
to 67.5%
Turnover
Medical Center
12.0%
Nursing 12.5%
2011 Goals:
Improvement in
access
60% new
patients seen
within
15 days
Improve patient
satisfaction
with:
Overall quality of
care
Overall
teamwork
between
2011 Goals:
Mortality rate
Improve to .70 of
expected
Indicators
Improve
Standardized
Infection Ratio to
1.11
Reduce adverse
events
to 7.67/1000
patient days
Achieve top
performance
2011 Goals:
Volumes meet
or exceed
budget for:
Hospital
discharges
55,085
Ambulatory visits
1,541,883
Surgical
operations
47,236
Achieve Medical
Center
Financial Targets
2011 Goals:
Demonstrate
results from
innovation
projects
Personalized
Medicine
Systems of Care
Value Based Care
Transformational Leadership
Strategic Planning (3)
26
doctors,
providers, nurses
and staff
Patient
engagement
in clinical
programs
Improve reliable
system
design and
communication
Develop quality
improvement
learning system
VUMC results of
operation
VUMC cash
savings
Cost per Visit
Cost per
Discharge
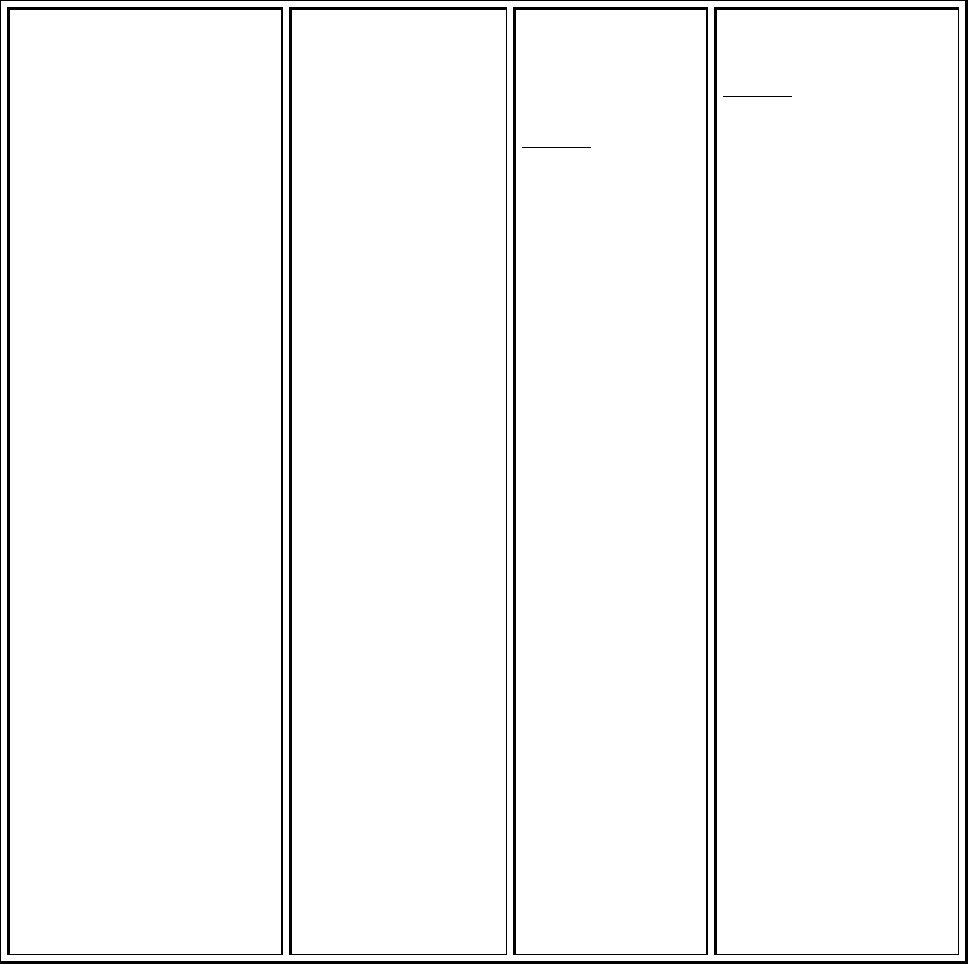
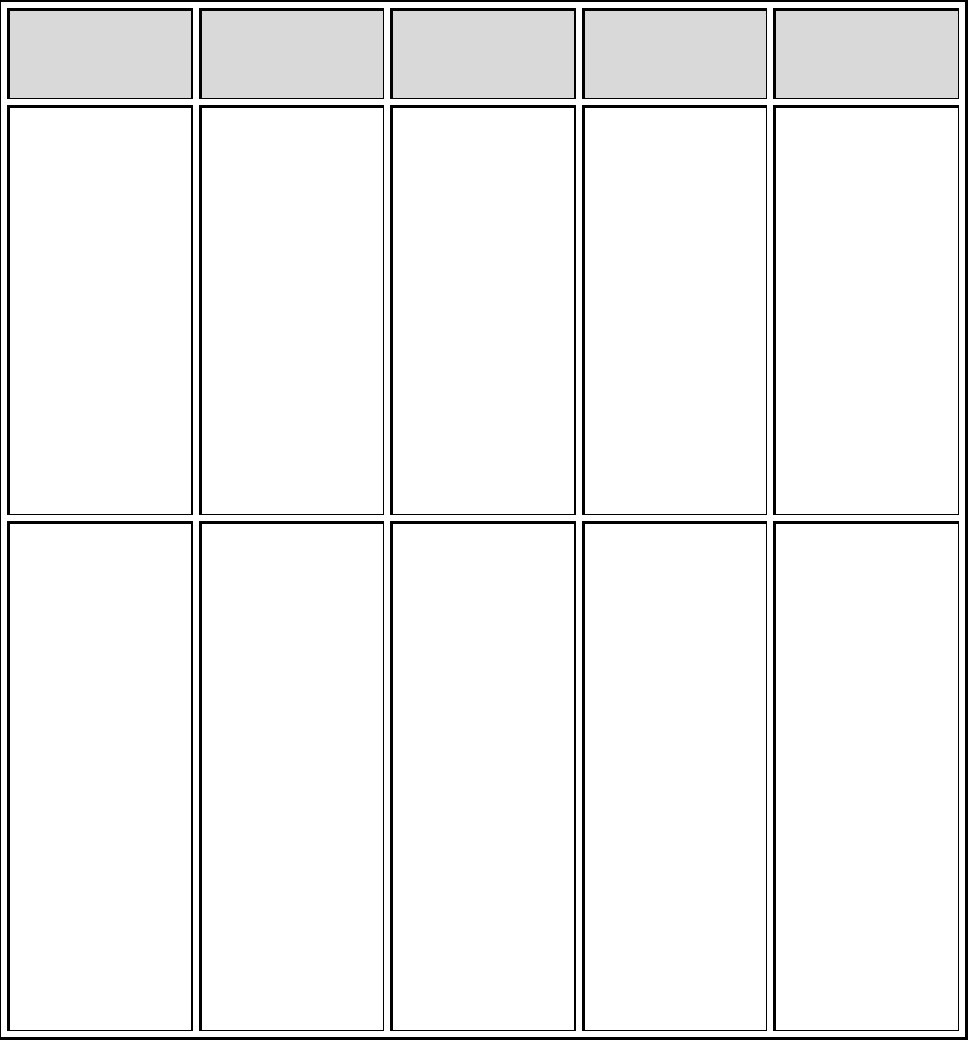
The structure used to develop and approve the pillar goals is demonstrated in Chart TL 3 - 2.
Chart TL 3 - 2: Figure Demonstrating structure and function for Vanderbilt University medical
Center Annual Pillar Goals
Structure: Board of Trust
Nursing membership: Chief Executive Nursing
Office is a member
Function: Approve Annual Pillar Goals
Structure: Medical Center Administrative Affairs
Nursing membership: Chief Executive Nursing
Office is a member
Function: Develop Annual Pillar Goals
Structure: VUMC Committees and Councils
(Examples: Quality Council, Compensation
Committee, Elevate Steering)
Nursing Membership: Nurses at all levels of
leadership - (Examples: Nursing managers,
nursing administrators, quality consultants
Function: Inform and recommend
p
illar
g
oals
Transformational Leadership
Strategic Planning (3)
27
Each Pillar is assigned to member of the Administrative Affairs team. The members of the
Administrative Affairs team include:
Vice Chancellor of Health Affairs
CEO of Vanderbilt University Hospital
CEO of Monroe Carrel Children’s Hospital
CEO of the Vanderbilt Medical Group - Service Pillar
Associate Vice Chancellor of health Affairs, Chief Strategic and Information Officer –
Innovation Pillar
Deputy Vice Chancellor of Health Affairs and CEO of Vanderbilt hospitals and Clinics –
Quality Pillar
Assoc. Vice Chancellor for Health Affairs & Chief Admin Officer
Associate Vice Chancellor of health Affairs and Senior Vice President of Finance –
Finance Pillar
Chief Executive Nursing Officer – People Pillar
These leaders then work through teams and committees focused on each pillar to
recommend goals for the coming year using historical performance data, external
benchmarking data and knowledge of organizational capability and capacity.
For 2011 pillar goal development, Marilyn Dubree, MSN, RN, NE-BC Executive CNO was
assigned to the people pillar. Marilyn was assisted by human resources experts in the
organization to identify strengths, weaknesses, opportunities and threats related to employees
and employment in healthcare in the Middle Tennessee region. Human Resources provided
knowledge of the regional human resource market supply and demand, compensation trends
and opportunities. The 2010 performance against VUMC goals for turnover and retention in the
Transformational Leadership
Strategic Planning (3)
28
first 18 months and the outcomes of the employee satisfaction survey were used to drive goal
development.
Through her work as the Executive CNO, Marilyn Dubree is responsible for the largest
subset of the workforce at VUMC. Throughout the year she works within the nursing structures
inclusive of the Nursing Executive Board and the Nursing leadership Board to optimize
performance in the people pillar. Marilyn has always focused on optimizing human
performance and thus organizational effectiveness and efficiency. To that end, Marilyn
developed approaches to comprehensively address human resource issues within nursing. This
effort, started several years ago is called “Be the Best, Keep the Best”. This is a nursing
approach led by Marilyn Dubree to select the right people, foster growth, address quality of
work life issues, and create the culture that retains the right people. Under the umbrella of the
Be the Best effort are several task forces. The task forces that make up that Be the Best team
are represented in Table TL 3-4.
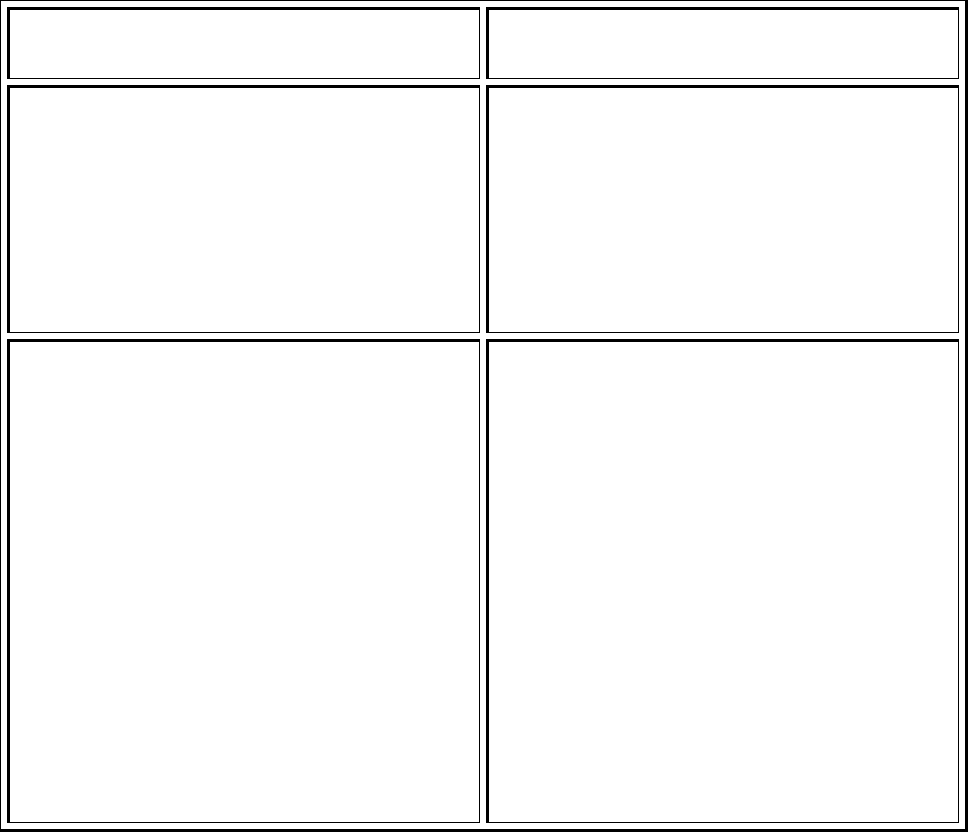
Table TL 3 - 2: Be the Best Task Forces and Purpose
Be the Best, Keep the Best
Task Force
Task Force Purpose
First Two Years Retention &
Recruitment
To assess, develop and implement effective strategies,
programs and processes for recruitment, selection,
orientation and support for nurses during their first two
years of employment at Vanderbilt University Medical
Center.
Clinical Work Force To identify, plan, recommend, and implement strategies
that:
Ensure resources and processes are in place to
appropriately deploy staff to meet organization,
unit/clinic goals of quality patient care and staff
satisfaction.
Promote and foster a dynamic staff and leader
partnership that promotes collaboration and
innovative problem solving of ongoing staff challenges
due to daily demand, new programs and overall
growth.
Transformational Leadership
Strategic Planning (3)
29
Diversity To cultivate an inclusive culture encompassing respect and
valuing individual uniqueness at all levels of Nursing
within Vanderbilt Medical Center
Leadership Development To identify, recommend, plan, and implement strategies
that will create an environment for nursing leaders that:
Supports excellence in clinical practice and customer
service
Enhances the work environment for staff and
leadership
Promotes professional and personal development of
staff
Fosters a workplace of participation and collaboration
Nurse Wellness
Develop programs and services based on the identified
needs of nurses
Advocate for the health & wellness of nurses
Evaluate programs and services based on indicators of
success
Serve in an advisory capacity to the Nurse Wellness
Program
Service improvement Identify and resolve issues hindering/preventing faculty
and staff from doing their bedside duties that ultimately
impacts meeting the needs of our patients and their
families.
Shared Governance
To evaluate and monitor the establishment of
purposeful shared decision-making structure within All
nursing patient care areas.
To promote and foster a dynamic staff-leader
partnership that promotes collaboration, shared
decision-making and accountability for improving the
quality of care, safety, and enhancing work-life
All of the membership of these task forces includes nursing managers and/or are lead by
nursing managers. For all groups there is a high level of engagement of staff nurses and
Transformational Leadership
Strategic Planning (3)
30
frontline leaders. These groups report their work, collaborate and inform Marilyn in monthly
“Be the Best” meetings. [TL3-Exhibit A-1-Be the Best Steering Committee Meeting Minutes] Be
the Best taskforce chairs share an annual report with all nursing leaders. The reports include
yearend accomplishments and proposed goals for the coming year. The nursing leaders at large
have an opportunity to influence the goals for the coming year at this meeting. Through this
work, Marilyn is fully knowledgeable and constantly engaged in understanding and managing
human resource issues, interventions and tactics that drive performance toward human
resource goal attainment. The “Be the Best” work informs her in a way that uniquely positions
her to lead the organization wide human resource goal development.
Accomplishments of these task forces listed in Table TL 3 -5 demonstrate how planning
has impacted efficiency and effectiveness within nursing.
Table TL 3 - 3: Accomplishments of Be the Best Keep the Best task Forces, 2009
Be the Best, Keep the Best
Task Force
Task Force Accomplishments
First Two Years Retention &
Recruitment
Set process in place to use peer interviewing for
placement of nurse residents
Revised nurse preceptor workshop based on focus
groups and implemented monthly as “Preceptor 1:
essential skills for the preceptor”
Developed plan for ongoing preceptor training – has
implemented: “Preceptor 2: communication skills for
the preceptor”
Offered unit based preceptor courses
Orientation and on-boarding of experienced nurses –
did a survey of experienced nurses who were within
their first 2 years of employment at VMC; CNO
breakfast w/ same population; complete a gap analysis
from feedback
Clinical Work Force
Improved nursing understanding of the need to take a
break by creating break buddy system on 7 RW,
creating charge nurse incentives n PCCU to encourage
nurses taking a break and Kay Stobaugh presenting
take a break success at April Fest
VMG Nursing Administration approved a policy for

Transformational Leadership
Strategic Planning (3)
31
Ambulatory Areas to Post Shifts and Fill with Available
Nurses from Other Areas. Staff are able to see needs
posted on the Nursing webpage and orientation plan
created to guide managers to ensure demonstration of
clinical competence of float nurses
System implemented for tracking of BLS certification in
Vandyworks (scheduling system) that alerts nurse and
manager near due date.
Diversity
Aprilfest 2009 Three one hour Cultural Workshops
Completed 7 One-Hour Cultural Workshops including
Lines of Communication: Interpreter Services at
Vanderbilt Dignity and Respect: Showing our Patients
Cultural Sensitivity, Generational Differences and
Healthcare Disparities for the Hispanic Patient.
Focusing on leadership development for diversity
leaders participated in “Attitudes Toward
Differences” workshops, completed Diversity gap
analysis of current practices and training for
leadership, developed a Diversity Web Site, developed
on-line Diversity Toolkit
Leadership Development
Developed behavioral rating tool to be used for
formative and annual evaluation of managers. The tool
clarifies the expectation of the competent, proficient
and expert manager and will help standardize
performance within established nursing manager
competencies
Nurse Wellness
Implemented Traveling Nurse Wellness Fair during
nurses week
Implemented “refresh rooms” in the critical care
towers to assist nursing in self-care activities during
work hours
Held an art retreat for high performing nurses
Completed Safety Walk to identify unsafe areas on
campus where nurses need to walk when traveling to
and from work locations
Transformational Leadership
Strategic Planning (3)
32
Increased the number of self-defense classes in 2009
Created and implemented “Flu Jail” to encourage flu
shots
211 new nurse case referrals to the Nurse Wellness
Specialist/EAP
Rounds made by NW Specialist to over 1000 nurses
during Nurses Week
Service improvement See TL3 EO
Shared Governance
Assisted Clinics transitioning to 100 Oaks to use
Shared Governance systems and processes for
transition planning
Launched VCH Float Pool and planning for a virtual
unit board
Verified staff involvement in Critical Care Tower
transition planning.
Shared Governance overview added to new program
aimed at developing leadership capability in Asst
Managers and Charge Nurses (“S3”)
The goals of these committees for 2010 calendar year are listed here that demonstrate a
continued focus on effectiveness and efficiency within nursing.
Table TL 3 – 4: 2010 Goals for Be the Best Keep the Best Task Forces
2010 Goals
–
Be the Best task Forces
First Two Years Retention & Recruitment
Use shared governance process to gather feedback and share information to achieve F2YRR
goals, include VPH
Improve communication between hiring official and recruiter throughout recruitment
process to on boarding
Maintain or improve selection/hiring process of new RN’s, including right person to the
right area/job
Conduct assessment of managers who currently use targeted selection and peer
interviewing – determine educational needs
Transformational Leadership
Strategic Planning (3)
33
Improve internal transfer process – review current policy and create career development
process to help guide nurses requesting transfers
Retain 87% of new nurses during their first two years at VMC
Implement Preceptor Nurse Alerts! and provide ongoing educational updates
Committee will review general on-boarding rounding tool that has been created and
determine need to revise current Nursing Rounding 30-90-180 tool
Complete assessment of educational needs of leadership teams in regards to retention and
socialization at the local level
Explore the pilot of the “Buddy System” implemented on 7N and determine feasibility of
rolling that system out to all units/departments
Clinical Workforce
Complete analysis of supplemental staffing needs for in/out patient areas
– Complete focus groups with in/out patient areas to assess need
– Review best practice and complete literature search
– Make recommendations for change in current process
Partner with Nurse Wellness Committee to educate and encourage breaks for staff
– Complete a literature search
– Pilot analysis of two units/clinics for times of no breaks/ no lunch
– Decrease no lunch Kronos punches by 25%
– Create a tool kit for managers and staff for education on importance of breaks
Implement education plan and formalize policy for floating nurses to OP areas
– Introduce floating option, educate on policy and process at VMG Managers Council
– Update Nursing Website for links to posted needs
Develop and Implement Subspecialty Nursing Fellowship
– Identify pilot area/ unit
– Create fellowship program as a gateway to subspecialty nursing
– Pilot fellowship will be designed and implemented in 2010
Add additional certifications for VandyWorks tracking and alerts
– ACLS, PALS, NRP, PEARS, and EOR
– Implement policy recommendations on certification expiration
– Attend Unit Boards to share information and Best Practice
Safety and Staffing
– Make recommendations for change in Schedule Process policy to support maximum
work hours per week
– Monitor data for rule enforcement of scheduled hours greater than hours per policy
– Review data with Workforce Planning Committee
Transformational Leadership
Strategic Planning (3)
34
Partner with other Be-the-Best Committees to improve satisfaction and strengthen the
retention of the experienced nurse
Nursing Diversity
Develop Diversity Ambassador Program Continue to collaborate with Recruitment on
diversity recruitment
MNPS Career Exploration Fair
Cultural Presentations for:
Martin Luther King Celebration
Aprilfest
Nurses’ Week 2010
Employee Celebration Month
Oktoberfest
Develop communication plan to advertise diversity website
Develop plan to increase number of subscribers to nurse alerts for diversity
Continue updates to website
Develop Cultural Awareness presentations for Medical Center Orientation and Nursing
Orientation
Support B-T-B Committees (Wellness, Leader Development and R2YR committees) in
advisory capacity
Participate in Black History Month Highlighting Nursing
Develop celebration months for other cultures
Collaborate with LDI, ODC and Nursing Education in an advisory capacity for development
of leadership support
Implement recommendations from Diversity Gap Analysis.
Develop on-line diversity training
Develop diversity training for leadership
Leader Development
Analyze current leader span of control at Vanderbilt
Compare staff satisfaction and turnover data and consider whether a correlation exists with
manager span of control
Compare Vanderbilt span of control with national statistics
Define specific performance behaviors related to job description evaluation scoring
Develop and implement communication plan
Collaborate with HR and Recruitment related to strategies for recruiting and retaining
managers
Transformational Leadership
Strategic Planning (3)
35
Collaborate with organizational initiatives focused on leadership assessment and
development
Develop collaborative working relationship with others in organization who are creating
leader development opportunities
Evaluate and revise existing leader orientation pathways
Nurse Wellness
Wellness Fair in 2010
Continue collaboration with Clinical Workforce, Diversity and Career Development re:
Maturing Workforce
Finalization of guidelines for Refresh Room
Additional performances of “Hey Florence”
Art Retreat for managers to reward high performers
Encore performance of Hey Florence
Compete plans for Refresh Rooms
Annual safety walk
Wellness Fair 2010
Continue partnerships with Professional Behavior Task Force, Occupational Health, and
VPD
Expand use of “Flu Jail” to encourage flu shots 2010
Increase self-defense classes to 1 per month
Improve Nurse Wellness page on website
Collaborate on ideas to increase presence of Nurse Wellness Program/EAP and other
resources to off-site staff
Continued website development
Increase communication about Nurse Wellness Program/EAP services to OHO and other off-
site staff
Encourage staff participation in Nurse Alerts
Shared Governance
Fall 2009 – Total Inpatient assessment (qualitative and quantitative).
Revamping of SG website and addition of “SharedGovernASK”
Partner with VMG training and development leaders
Bylaws Convention
Virtual Unit Boards
Dissemination of inpatient Unit Board assessment data
Next Nursing Staff Summit
Partnership with other BTB Committees
Transformational Leadership
Strategic Planning (3)
36
Shared Governance Traveling Fair
Coordination with Nursing Leader Development using SG as foundation in building leaders
Coordination with Nursing Research Committee in evaluating effectiveness of Shared
Governance
Coordination with NEB in developing future nursing org structure
Coordination with either Retention Committee or Mature Workforce Committee regarding
experienced nurse data and action plan
[TL3-Exhibit-A-2-Be the Best 2009 Annual Report]
Entity Planning Structures and Processes and Nursing Effectiveness and Efficiency
Each entity (VUH, VCH, VPH, Clinics) has planning processes annually as well. There is a
great amount of nursing influence in these planning processes. The evidence in this section
demonstrates the nursing influence in all entities.
Annually, Larry Goldberg, the CEO of Vanderbilt University Hospital (VUH) leads a
planning effort with the VUH team. Among others, the VUH planning team includes, Pam Jones,
RN, MSN the CNO of VUH, Nancy Feistritzer, RN, MSN the Associate Director of Perioperative
Services, and Robin Steaban, RN, MSN Administrator for Operations and Nursing in the
Vanderbilt Heart and Vascular Institute. These nursing leaders develop the VUH plan with other
non-nursing leaders. A full review of the year end 2010 VUH Operating plan is provided. In
addition, Robin Steaban leads the development of the VHVI operating plan. Examples of some
operating plan elements that have improved efficiency and effectiveness are in the Table TL 3-7
below.
TL 3 – 7: Examples of VUH Operating Plan Examples
FY 2010 Goal Responsible
Person
Impact on Efficiency and Effectiveness
Goal was to decrease
infant mortality by
predicting high risk
Robin Mutz RN,
MBA
Administrative
Improved efficiency of utilization of ultrasound
machines. Center for Women’s Health consolidated and
moved 3 clinics to the One Hundred Oaks location in Feb.
08. At that time we were operating 3 ultrasound
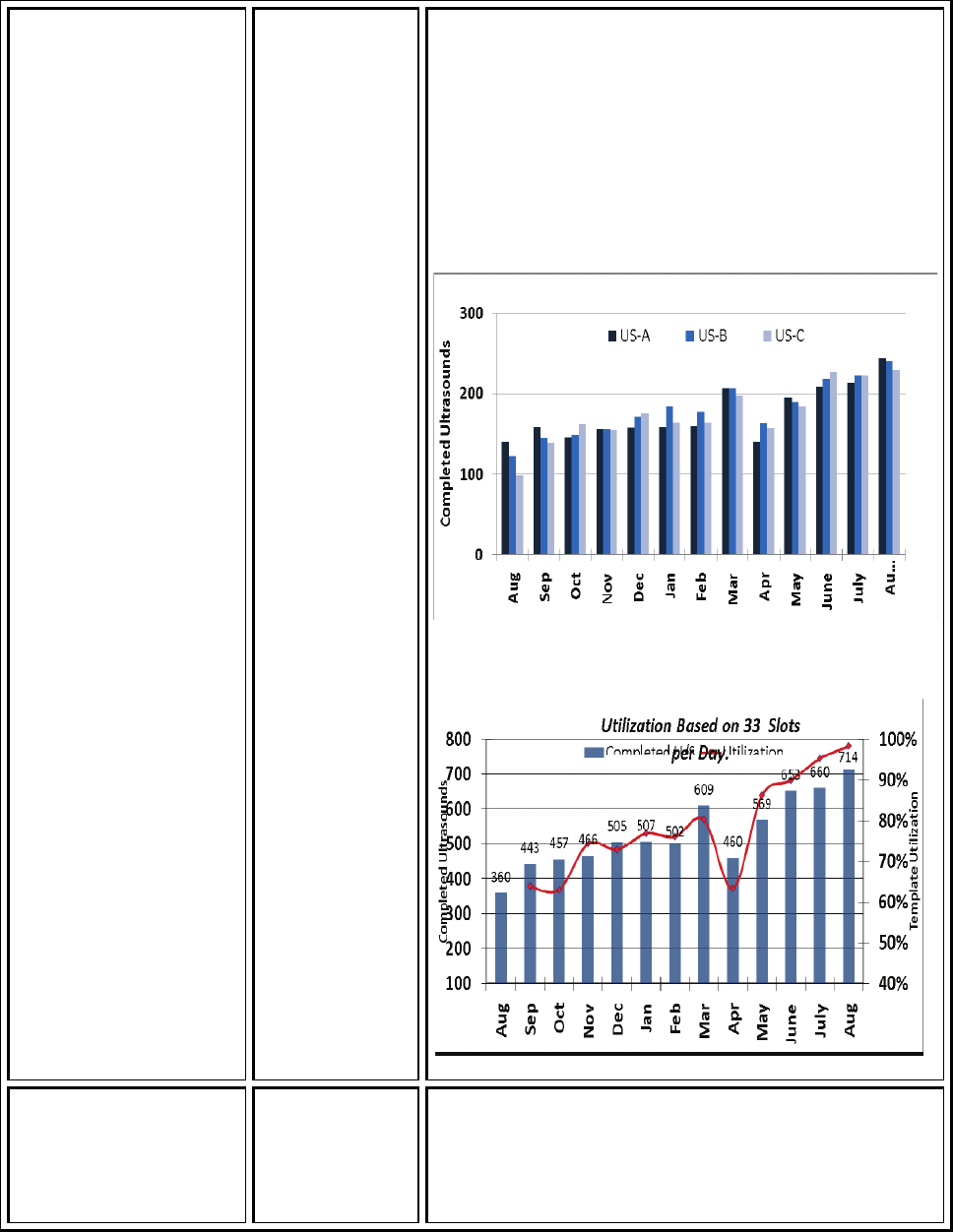
Transformational Leadership
Strategic Planning (3)
37
pregnancies. This
required increasing the
utilization of
ultrasonography for
early identification of
high risk infants in the
face of fixed resources.
Director,
Women’s
Health
machines at less than 50% capacity. Through redesign
efforts, we smoothed the template for each machine,
evened the schedule for each machine and gave the
sonographers daily targets for numbers of completed
scans (33 is the goal). We also adopted a philosophy of
“just say yes” whenever they were asked to do a scan.
Through the efforts, we are now at 98% increase over
the same month last year. The graph is attached.
Implement Central
telemetry monitoring
for 9 North, TVC
observation and 15
Robin Steaban
RN, MSN,
Administrator
New telemetry equipment implemented and
Central monitoring expanded to include 9 North, 7
RW, ED. This improves the monitoring accuracy
within the organization by centralizing observation
Transformational Leadership
Strategic Planning (3)
38
beds in the ED VHVI of cardiac rhythms to highly trained sta
f
f. It also
consolidated the human resources to one area. .
The telemetry tech pool was large enough to cover
all unexpected call outs with telemetry techs
instead of nurses as was the norm in the
decentralized model.
Integrate Vascular
patient population into
the VHVI inpatient bed
allocation and service
Robin Steaban
RN, MSN,
Administrator,
VHVI
Vascular patients integrated into VHIV consolidating
vascular patient with nursing experts in CV care.
Nurses focused only on CV patients and working
with the same MD teams everyday are able to more
effectively care for patients and ensure patients
move through the system with accuracy and
efficiency.
Develop Quality
Council leading to
development of a
forum for review of
near misses and
failures in the
Vanderbilt heart and
Vascular Institute
Robin Steaban,
RN. MSN
Administrator
VHVI and
Brittany
Cunningham,
RN, MSN,
Quality
Consultant,
VHVI
Development of ImPaCT
–
Improving Patient Care
Together – See full story below
VUH leaders also meet monthly to review and influence Informatics priorities.
“IMPACT” in Vanderbilt Heart and Vascular Institute (VHVI) – In Support of the Quality Pillar
Goal
In 2009, VHVI chartered a Quality Council. The Council membership includes all nursing
managers, VHVI Medical Directors and Administrators and is focused on meeting the quality
Pillar goals developed by the organization. While the Council has proven to be an effective
forum for quality improvement planning, outcome review and tactical planning, the need was
identified to develop a system and process to learn more quickly from near misses and harm to
Transformational Leadership
Strategic Planning (3)
39
patients. This is consistent with literature on Highly Reliable Organizations where one
characteristic is pre-occupation with failure.
The idea was to create a forum to improve the timely and effective review of cases so
early correction in systems and processes could be made to prevent harm in other patients.
Robin Steaban, RN, MSN, the administrator for VHVI, supported the efforts of Brittany
Cunningham, RN, MSN, VHVI Quality Consultant Jeff Boord MD, the Quality Director and Tom
DiSalvo MD, the Quality Medical Director for VHVI, as the idea of a team that met regularly to
focus on near misses and harm was envisioned and eventually created. Through the work of
this team Managers, Medical Directors and Administrators gathered and chartered the group
which eventually became known as ImPaCT or Improving Patient Care Together.
The goal of the ImPaCT effort was to craft a sustainable management process for CQI for
all clinical operational units of the Vanderbilt Heart and Vascular Institute. It was the aim to
create a safe environment where incidents could be shared and learned from. The work was
based on the belief that continuous quality improvement (CQI) in health care systems
necessitates an approach to review of:
Care delivery processes
Systems
Group and individual performances
Incidents
Outcomes
VHVI leadership believed a robust process should be:
Multidisciplinary
Occur in “real-time”
Provide detailed review and discussion of care processes, performance and outcomes
Generate actionable rapid cycle improvement opportunities
A standing interdisciplinary biweekly managerial forum (ImPaCT- “Improving Patient
Care Together”) of quality medical directors, key clinical physicians and nurses, nursing unit

Transformational Leadership
Strategic Planning (3)
40
managers, hospital administrators and quality consultants was developed. The meeting
follows a standing structured agenda:
All mortalities since last meeting
Morbidity including “major misses” and major adverse events
Rapid response team calls
Out of ICU “codes”
Events reported by staff in our institutional incident reporting system
Events or issues brought forward by any clinician or unit manager
Interval progress on ongoing rapid cycle improvement projects
ImPaCT acts as the interchange for quality and safety information and provides the following
functions.
Adverse events and patient safety issues are discussed in a confidential forum that
promotes Problem solving and accountability but avoids blame
ImPaCT can identify events that merit root cause analysis, and also follow up on the
findings
ImPaCT coordinates communication and process improvement efforts with other
departments
ImPaCT develops and prioritizes quality improvement initiatives
The forum allows the exchange of information between many groups looking at near
misses and errors. It provides a forum for closing the loop on issues raised in other forums as
the members are operationally and clinically focused. A graphic of the information flow
between teams is depicted below.
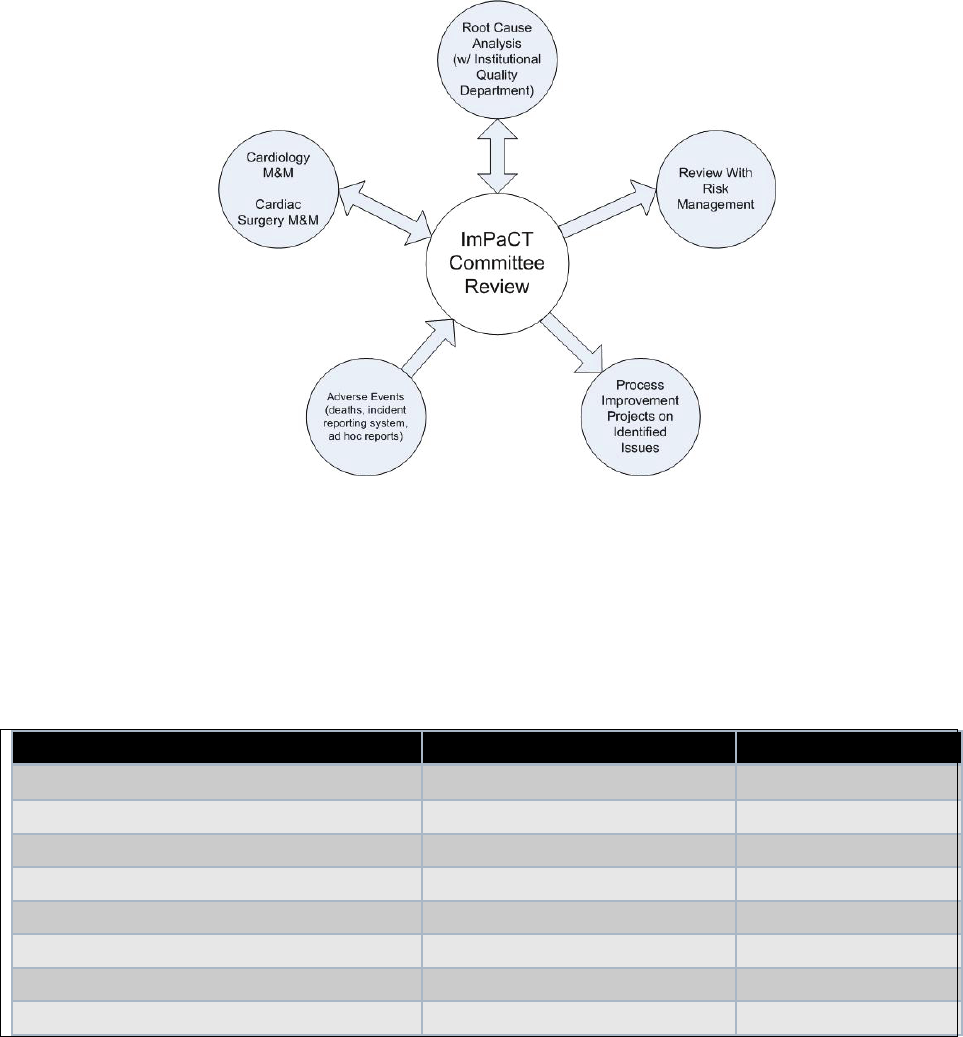
Transformational Leadership
Strategic Planning (3)
41
In the first year various types of issues have been brought to this forum. The issues
identified that required action were categorized and quantified below:
Table TL 3 – 8: Issues Requiring Action
Topics Contribution (N) Percent
Handoff and Communication 13 28%
Medicine Administration 10 22%
Equipment 7 15%
Transport of Patients 5 11%
Education back to staff (i.e. M & M) 4 9%
Risk Management Cases 3 7%
Blood administration 2 4%
Vascular Surgery Integration 2 4%
The examples of Quality projects that resulted for the IMPACT review include:
Development of ICU “transport time out” to improve safety of patient transport
Development of standardized nurse report form for patients transferred in from an
outside facility
Transformational Leadership
Strategic Planning (3)
42
Implementation of a rapid nurse debriefing process to identify and capture key data
related to patient falls
Implementation of a handoff process for patients with an indwelling vascular sheath
after catheterization
Training on communication of adverse outcomes and errors for unit nurse managers
In conclusion, a multidisciplinary, structured, regularly scheduled meeting of physician
and nursing leaders, unit managers, and administrators is a critical component of performance
management and improvement. This forum not only facilitates learning and collaboration
between clinical areas, but also creates a culture of safety and enhances communication.
[TL3-Exhibit-B-1-QCO ImPact Conference Poster]
Revision of Operating Room Case Cart Operations and Supply Management
Lead by Nancye Feistritzer RN, MSN, Associate Hospital Director, Perioperative Services
In November 2009, we opened a new Critical Care Tower which included 141
New acute-care inpatient rooms and 12 new state-of-the are operating rooms, and is the most
significant increase in adult inpatient hospital rooms at VUMC since it’s opening in 1980. In
order to support the opening of the Tower, VUMC’s Medical Center Support Services (MCSS)
worked with a logistics consultant to redesign the current state of materials management and
case cart delivery as it services the preoperative environment.
Findings from the original assessment were divided into two broad categories: Case
Management operations and Supply Operations. Through extensive interviews, observation of
current operations and data analysis, teams focused recommendations on these categories in
three (3) areas:
1. People
Training staff and managers to develop and use standard policies, operating and
reporting procedures
2. Process
Transformational Leadership
Strategic Planning (3)
43
Streamlining current operations to be more efficient and produce more consistent
results
3. Technology
Realigning technology to better support current and future processes. In addition,
multidisciplinary teams worked with MCSS to design and construct a new offsite
Case Cart Operations Center. The new Case Cart Operations Center was built in
Briley Park and was put into operation in November 2009. This facility replaced the
majority of the current Central Supply, freeing up valuable storage space at VUH for
a large percentage of the cases currently performed. With few exceptions, case carts
will be processed at the CCOC. Case carts fall into one of three categories:
Scheduled elective and add-on case carts delivered multiple times per
day
Specialized pre-built trauma supply totes and VUH pre-built instrument
cart, maintained at VUH and replaced by CCOC as used
POD specific “specialty” carts, managed at par levels and replenished
daily
Carts that are not case specific but are managed through the Central Supply staff (e.g.
isolation carts) continue to be managed via the VUH Central Supply.
Improvements
The following areas were identified during the assessment phase, redesigned and
implemented during the course of the entire project.
Case Management/Perioperative Improvements:
Established Preference Card Maintenance policy and SOP. In addition created charter
for Preference Card Review Group which will meet regularly to establish standards and
approve changes.
Established Weekly, Monthly and Quarterly OR Management Reporting. Scheduling
Accuracy as well as other performance metrics established and placed on OR Dashboard
Transformational Leadership
Strategic Planning (3)
44
Established standard scheduling policies and SOP and it relates to the CCOC
Reviewed and presented case “add-on” procedures and management of surgical block
time. Presented data findings to leadership to aid in operational decisions, i.e. case
block release times
Created specialty supply and room stock carts to eliminate inventory in multiple bulk
locations. (12) Specialty supply carts were created for key service lines and placed in
strategic locations. Carts containing basic room stock were also created and placed in
each room. These carts are replenished daily and reduce duplicate inventory as well as
reduce clinical involvement in supply chain functions.
Perioperative IT Improvements:
Implemented requirements for all non-emergent appointment requests through
STARform interface
Reviewed and made suggestions for standard reason codes
Case Cart Process Improvements:
Established standard “home” locations for all instrument trays
Established standard case cart build SOP
Established supply “stay/go”, identifying which supplies remain at VUMC and which
move to the CCOC freeing up much needed support space at VUMC
Establish a policy and SOP for communication between Central Supply and OR for
missing supplies and instrument trays on case carts
Establish policy and SOP for communicating missing supplies, instruments and other
items on Preference Card
Case Cart Information Technology Improvements:
Revised use of PMM Pick Ticket to support Point-of-Use technology and preference card
clean-up
Transformational Leadership
Strategic Planning (3)
45
Prepared operations for Point-of-Use Technology
Established surgical instruments “stay/go” list indentifying instrument sets thatshould
stay and be processed at VUMC and sets that should be moved and be processed at the
CCOC
Instrument Processing Improvements:
Established a policy and SOP for more strategic use of Censitrac to support off-site case
cart operations
Established a policy and SOP for determining instrument processing priority
Realigned shift schedules to more align with the needs of the medical center
Establish policy and SOP for identifying tray processing location
Establish a policy and SOP for identifying critical (show stopper) instruments for each
instrument tray
Implemented quality control measures to ensure all instruments are sterilized
Instrument Processing Information Technology Improvements:
Realigned instrument scan points
Established management reporting for KPIs
Rolled out interface between Censitrac and ORMIS schedule
In conclusion, the design and creation of the Case Cart Operations Center brought
together interdisciplinary team of nursing leaders, front line nursing staff, administrators,
physicians, and front line support staff to review, change and create new procedures and
protocols that allowed case cart operations to be moved offsite.
Some production statistics:
Transformational Leadership
Strategic Planning (3)
46
Case carts processed: 2,100/month
Instruments processed: 420,000/month
Case cart supplies picked: 70,000/month
[TL3-Exhibit-C-1-Case Cart Current Performance]
Transformational Leadership
Strategic Planning (3)
47

Transformational Leadership
Strategic Planning (3 EO)
48
Strategic Planning
Source of Evidence 3 EO
Describe and demonstrate the outcome(s) that resulted from the planning described in TL 3.
Strategic planning and operational planning drive Vanderbilt nursing’s agenda each year.
Below are three examples of outcomes that have resulted from planning. They include; Nurse
Residency, Door to Balloon SWAT team and MyHealth@Vanderbilt.
Strategic Planning for Needed Nursing Resources - VUMC Nurse Residency Program
Background
We have had significant growth in patient volumes over the past five years. As the Nursing
Executive Board and other hospital leaders engaged in a strategic planning process for the
Critical Care Tower it became evident that there would need to be a more robust mechanism
for attracting and retaining qualified nurses to meet the increased capacity. After one and a
half years of planning, the consolidated VUMC Nurse Residency Program (NRP) was launched in
July 2008 by the Department of Nursing Education and Professional Development as part of a
strategic approach to recruitment and retention of staff. The program was designed to meet
the strategic need of recruitment by standardizing the application, interviewing, hiring, and on
boarding process. The new program was marketed through the Vanderbilt Nursing website
(see Figure TL 3 EO – 1 below). The strategic need of retention was addressed by developing a
program to help novice nurses successfully transition from the student nurse role to the
professional nurse role, increasing satisfaction and decreasing the turnover rate of those new
graduates.
The program at VUMC, is affiliated with the University HealthSystem Consortium (UHC) and
the American Association of Colleges of Nursing’s Post-Baccalaureate Nurse Residency
Program. The residency is a year-long program, which consists of orientation specific to
graduate nurses, as well as seven-weeks of core and track orientation during a rotational phase,
followed by a match to a permanent unit. Once matched, the program co-leaders mentor the
new nurses and lead eight monthly facilitated workshops conducted during the first year of
employment. Additional details of the NRP are outlined on our Nursing website at
www.vanderbiltnursing .com with a direct link:
http://www.mc.vanderbilt.edu/root/vumc.php?site=vanderbiltnursing&doc=9935
Transformational Leadership
Strategic Planning (3 EO)
49
Participants
The planning committee for creating the consolidated NRP was diverse with nurse
educators, and managers who represented all inpatient nursing areas of VUMC and nurse
recruiters and administrators from Nursing Recruitment and Human Resources. The members
of the Residency Planning Committee included the following:
Table TL 3 EO – 1: Residency Planning Committee Members
Debbie Arnow, MSN, RN, NE-BC
Director Clinical Education and Professional Development
–
Children’s Hospital
James Barnett, MSN, RN Nurse Educator
–
NCU
Richard Benoit, MSN, RN Nurse Educator
–
SICU
Cindy Brown, RN, MSN MCE OR Director
Ed Dennis, MSN, RN Nurse Educator
–
Burn Unit
Tracey Fargo, BSN, RN Nurse Recruiter
–
HR
Elizabeth Fritz, MSN, RN Nurse Educator
–
Labor & Delivery
Kara Gordon, MSN, RN Nurse Educator
–
MICU
Todd Griner, MSN, RN, NEA-BC Manager
–
10S
Rachael Hamilton, BA Administrative Manager
–
Nursing Education and
Professional Development
Beth Hodge, MSN, RN Nurse Educator
–
3 and 5/6 RW
Collette Judd Recruiter
–
HR
Erin Kuhn, MSN, RN Nurse Educator
–
Perioperative Services
Anya Lockert-Young Recruiter
–
HR
Lori Martin, BSN, RN Nurse Educator
–
VUH ED
Leanna Miller, MSN, RN Nurse Educator
–
Trauma
Amy Moore, BSN, RN 3, CEN,
EMT, IV
Flight Nurse - LifeFlight
Nancy Moore
–
RN 7RW
Christy Mullen, BSN, RN Nurse Educator
–
NED VCH
Rosalyn Norris HR Recruitment
Cathy Ollom, MSN, RN Nurse Educator
–
Oncology
Terry Owens Program Coordinator
–
Nursing Education and Professional
Development
Shelly Padgett, BSN, RN Nurse Educator
–
Cardiology
Debianne Peterman, Ph.D., MSN, Director
–
Nursing
Transformational Leadership
Strategic Planning (3 EO)
50
RNC-NIC, NE-BS Education and Professional Development
Sheryl Redlin-Frazier, BSN, RN Nurse Educator/Assistant Nurse Manager, 4 E
Laurel Roberts, BSN, RN Administrative Director
–
VCH
Donna Ruth, MSN, RN Nurse Educator
–
Labor & Delivery
Teresa Simpson, BSN, RN Nurse Educator
–
CVICU
Sherri Stringfellow Art Director - Nursing Education and Professional
Development
Martha White, MSN, RN Nurse Educator
–
9N & 9S
Bridgette Willette Director HR Recruitment
Chris Wilson, MSN, RN-BC Director Clinical Education and Professional
Development - Nursing Education and Development
Sandra Winfield Recruiter
–
HR
Methods and Approach
The committee reviewed historical data that identified a turnover rate for first-year
nurses that was typically very high and very expensive to the medical center (35-55%) and
developed a program with the hypothesis that the turnover rate of this population would be
reduced by employing a standardized nurse residency strategy. Working with HR and assigning
one Nurse Recruiter (Tracey Fargo, BSN, RN) who would serve as the recruitment liaison for this
program helped to organize the marketing and recruitment efforts.
Tracey conducted onsite visits to local schools of nursing and sent out email marketing
blasts to schools around the country at the time that we posted the NRP positions. We created
an introductory video and placed all information on the Nursing website. A series of town hall
meetings were conducted to inform current VUMC staff of the changes we were making to the
hiring process for graduate nurses. We set up one portal of entry for all of the applications to
enter into the system and created and built an NRP-specific database that allows us to send out
standardized communication to all candidates during each phase of the inquiry, application,
interviewing, and hiring process.
An example of the marketing approach to this project through the website can be seen in G
raph TL 3 EO - 1 below.
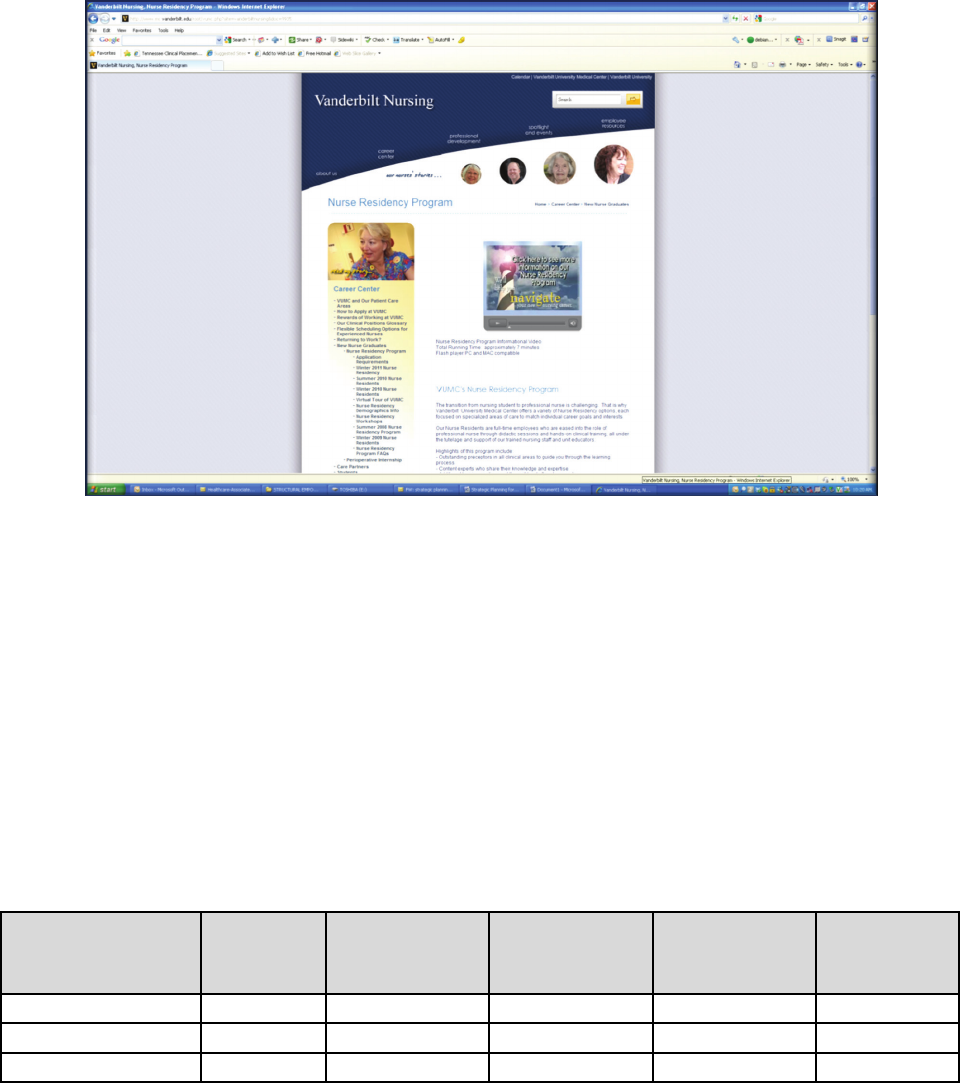
Transformational Leadership
Strategic Planning (3 EO)
51
Graph TL 3 EO – 1: Nursing Website Nursing Residency Program
Outcomes
The strategic objective of attracting qualified applicants has been successfully achieved.
The [TL3EO-Exhibit A-1-Nurse Residency Summary Report] shows the number of applicants for
each cohort. We have been able to attract a diverse group of graduate nurses from thirty-nine
(39) states plus DC with a 176 different nursing programs represented. Our average GPA is 3.43
(on a 4.0 scale) with each cohort. The percentage of graduates with BSN degrees has increased
since the initiation of this program and our average now is at 80%. Our retention rate of these
new graduates has improved significantly as indicated by the table below.
Table TL 3 EO – 2: Retention Rates of Nurse Residents
Cohort
3 months
6 months 9 months 12 months
>12 mos.
and < 24
mos.
Summer 2008
100%
97.1% 96% 91%
85%
Winter 2009
100%
98.8% 95% 92%
92%
Transformational Leadership
Strategic Planning (3 EO)
52
Evaluation:
It is clear from the data above that this program achieved both strategic objectives of
recruiting a ready supply of highly qualified nursing staff and retaining those nurses at VUMC.
Door to Balloon Time SWAT Team
Purpose/Background
The goal established by the American Heart Association/American College of Cardiology
for patients experiencing an acute MI was to have the culprit artery opened and blood flow
restored to the heart within 90 minutes of patient presentation to the ED. There has been a
long standing collaborative effort between the ED and the cardiac cath lab to achieve that goal.
In 2008, the Chest Pain Center Committee identified the need to improve the door-to-balloon
time for patients experiencing ST elevation myocardial infarction (STEMI), particularly in
regards to the interval from activation of the cath lab until the patient arrived to the lab.
During off hours (evenings and weekends), a call team responded from outside of the
hospital with a 30 minute maximum response time and this was identified as the primary
limiting factor to improvement. Some staff members lived in a range that allowed them to
respond to a page for an acute MI and be on site within 30 minutes but not faster. The patient
could not be moved to the cath lab without staff. This fact delayed the actual intervention time
because staff reported to Vanderbilt, went to the lab to prepare the area and then retrieved
the patient. The median time the patient was moved from the Emergency Department to the
Cath lab was 37 minutes. This left only 52 minutes for the patient to be prepped, the MD to
gain arterial access, complete a diagnostic cath and re-vascularize the culprit vessel. The
interval time of patient arrival to transport to the cath lab needed to be shortened.
Methods
The CVICU Manager met with charge nurses of the CVICU to develop a plan for the
charge nurse to be involved in the care of acute MI patients. The plan developed was for the
charge nurse to respond to a “STEMI Alert” page by going to the ED. Once there, the patient
would be prepped and the ED nurse, cardiac fellow and CVICU nurse would transfer the patient
to the cath lab and prepare them for the procedure by getting the patient on the cath table,
connect the patient to the defibrillator pads, connect cath lab monitoring equipment and
provide care until the cath lab team arrived. The roles and responsibilities of the ED staff and
the cardiac fellow were also more clearly determined.
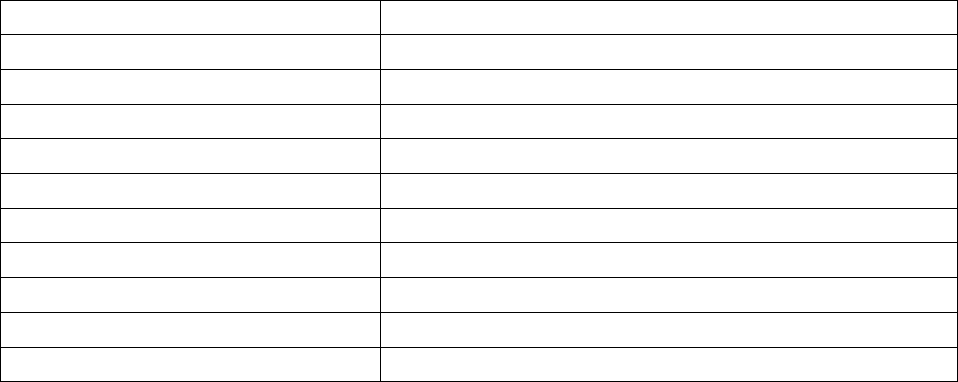
Transformational Leadership
Strategic Planning (3 EO)
53
Once requirements and resources identified (CVICU Charge Nurse), protocols were
developed. The team identified training needs of the CVICU charge nurse as response/cardiac
catheterization environment. The CVICU Charge nurse would have to work in an environment
where they were unfamiliar. There were competency requirements established and formal
training and competence validation. A medication box was developed in collaboration with the
pharmacy for administration of emergency meds during time the CVICU nurse would be in the
lab. In addition, a fully implementable contingency plan had to be developed in case the charge
nurse was unable to leave the CVICU because of acuity or other situation.
After implementation, the median transfer time decreased to 30 minutes and has been
sustained.
Table TL 3 EO – 3: Participants
Jeannie Byrd, MSN, RN, NE-BC CVICU Manager
Janice Sisco, BSN, RN ED Manager
Laura Zelenak, RN, Cardiac Catheterization Lab Manager
Tiffany Richmond, RN Cardiac Catheterization Lab Assistant Manager
Carol Parsons, RN Cardiology Case Manager
Brittany Cunningham, RN, MSN Quality Consultant
Kathy Burns, Med, RN, CCRN CVICU Clinical Nurse Specialist
Dan Johnson, Dph Clinical Pharmacist
Michelle Hasselblad, BSN, RN Director, Cardiac OR and Catheterization Lab
David Zhao, MD Cardiac Catheterization Lab Medical Director
Thomas DiSalvo,MD VHVI Quality Director
The workgroup implemented this change for of the D2B Swat Team in January 2008 and
the evaluation follows.
Evaluation
There is an analysis of every STEMI patient coming through the ED. Interval
measurements were established for each segment of time dependent care. Median time of
transfer decreased from 37 minutes to 30 minutes. This has been sustained since the
implementation of the process. [TL3EO-Exhibit B-1-D2B Swat Team Policy, TL3EO-Exhibit B-2-
CPC Meeting Minutes]
Transformational Leadership
Strategic Planning (3 EO)
54
My HealthCareTeam@Vanderbilt
Purpose/Background
A study was done through the electronic medical record that demonstrated a large
number of patients with hypertension, diabetes, and/or heart failure whose conditions were
not under control. Vanderbilt set a goal to improve the health of this population and to try to
prevent costly ED visits and hospitalizations that could be avoided by improving primary care
access and follow-up. [TL3EO-Exhibit C-1-Summary Presentation]
VUMC provided an innovation grant to create a “medical home” within our primary care
practices to care for patients with hypertension, diabetes and/or heart failure in a manner that
would get their chronic conditions under control and try to reduce morbidity and mortality and
prevent unnecessary emergency visits and hospitalizations. The medical home would make use
of RN “care coordinators” to implement evidence-based, protocol-based individualized care
plans.
Methods/Approach
An interdisciplinary group took several months putting together the proposal for the
project. They researched the evidence for reducing mortality and morbidity of the three chronic
conditions by providing close follow-up, coaching, goal setting and behavior modification by
registered nurses working with the primary providers to develop individualized evidence-based
care plans for each patient. The project was then funded.
The specialists, for example the heart failure nurse practitioner, Connie Lewis, RN were
engaged to write care protocols. A dashboard was built to show the progress and care needs of
the patients. Care plans were developed and placed in into StarPanel, the EMR system. RN Care
Coordinators were hired. Data definitions (defined what “being in control” and “at target”
means) were developed. Measures were built into the EMR.
A system to stratify patients was created and the team began enrolling patients.
The primary care practices’ patients were stratified by co-morbidity, and patients were enrolled
in the proof of concept project, so far involving 3 primary care physicians, their care teams, and
2 RN care coordinators.
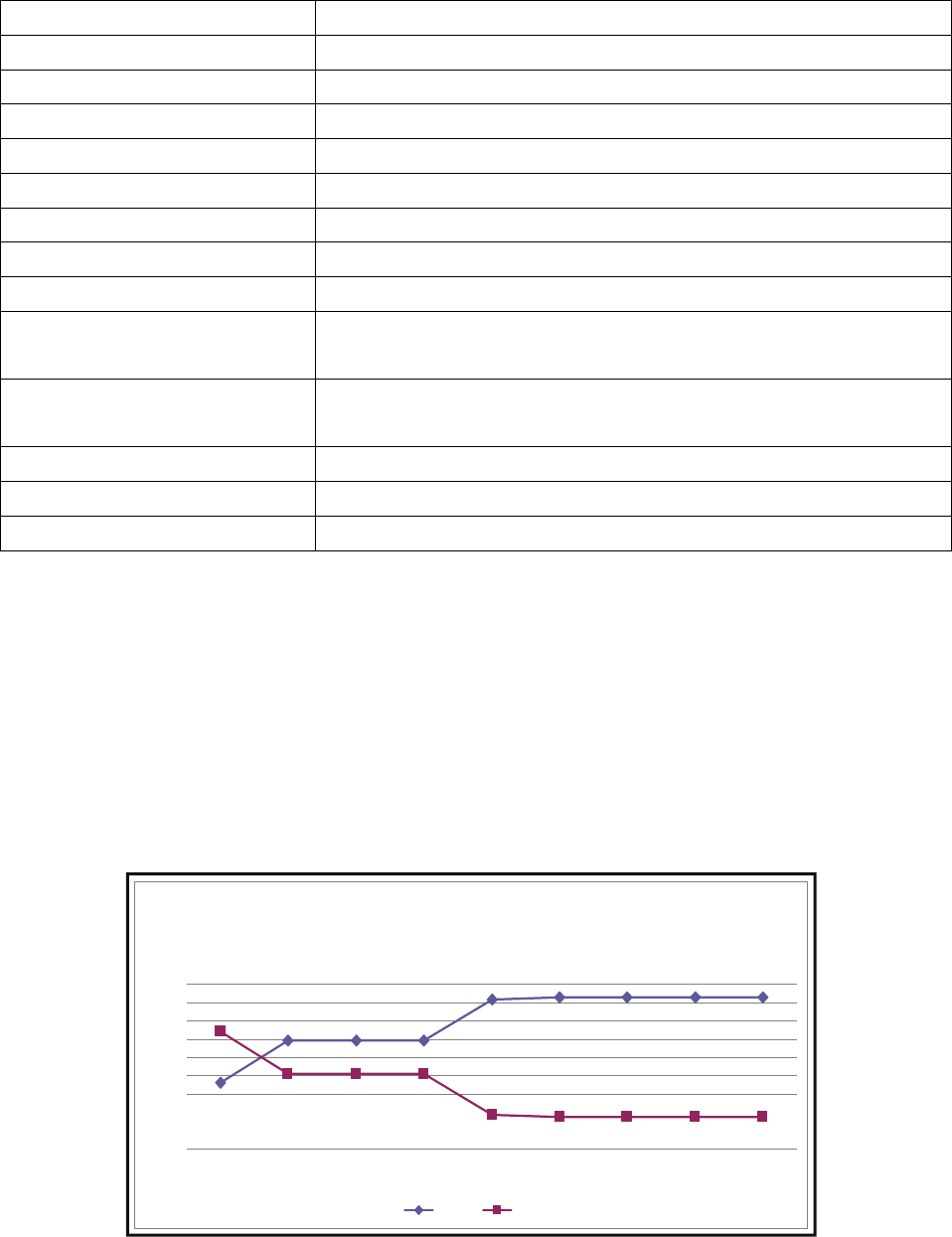
Transformational Leadership
Strategic Planning (3 EO)
55
Table TL 3 EO – 4: Participants
Jim Jirjis, MD, MBA Primary Care physician, Lead, Main Campus
Ralf Habermann, MD Primary Care Physician
Jim Powers, MD Primary Care Physician
Bill Gregg, MD Primary Care Physician, Informatics
Pete Powell, MD, MBA Primary Care Physician, Lead, Williamson Co.
Racy Peters, RN, MSN VMG Associate Director, Operations
Betty Akers, BS Business Administrative Director, Primary Care, Operations
Pat Covington, BSN, RN, CRRN Clinic Manager, Operations
Anne Hurd, RN Clinic Nurse
Julie Scott, BSN, RN Manager, Center for Disease Prevention, Care Coordination
Management
Sharon Mullins, RN Health Information Systems Project Manager 2, Project
Manager
Joan Peterson, RN, CCM, CDE Care Coordinator
Rebecca Bumm, RN Care Coordinator
Collin Mothupi Quality Value Analyst
Outcomes/Impact
The data demonstrates the program and nursing interventions are improving patient’s
control of chronic conditions. There is insufficient data at this time to determine whether
incidence of ED visits or hospitalizations is affected. [TL3EO-Exhibit D-1-MHTAV Work Plan]
Hypertension control improved after the intervention from the MyHealth@Vanderbilt team.
Graph TL 3 EO – 2: Hypertension Measure
Hypertension Measure
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Basel ine 2-Jun 14-Jun 28-Jun 14-Jul 27-Jul 2-Aug 8-Aug 16-Aug
IC + IT OOC
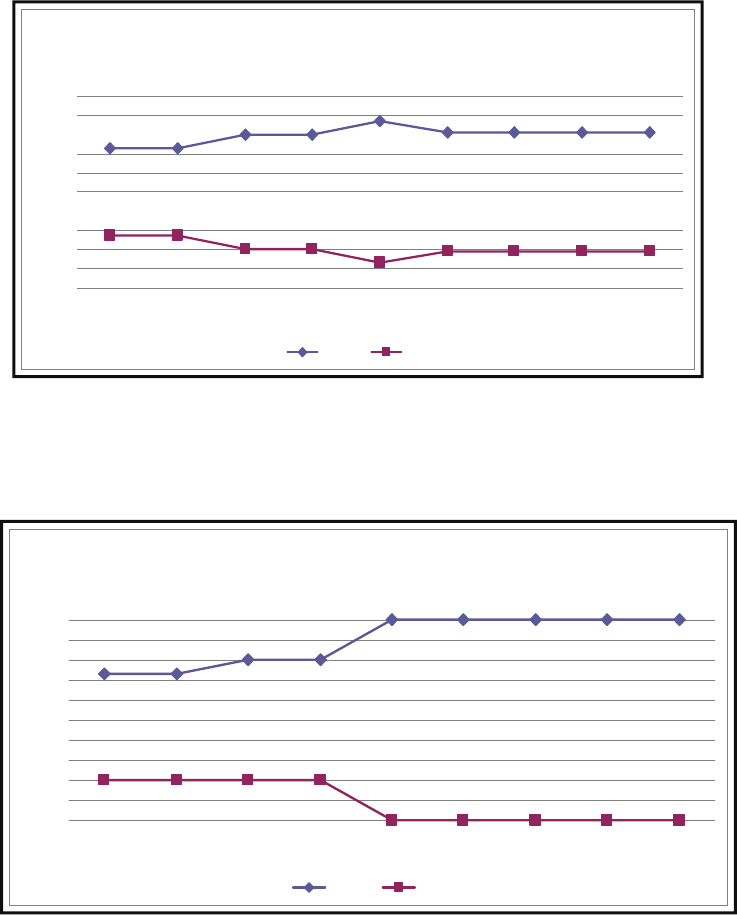
Transformational Leadership
Strategic Planning (3 EO)
56
Graph TL 3 EO – 3: Diabetes Measure
Diabetes Control improved after intervention from the MyHealth@Vanderbilt Team
Graph TL 3 EO – 4: CHF Measure
Control of HF improved after MyHealth@Vanderbilt team interventions
Diabetes Measure
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Baseline 2-Jun 14-Jun 28-Jun 14-Jul 27-Jul 2-Aug 8-Aug 16-Aug
IC + IT OOC
CHF Measure
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Basel ine 2-Jun 14-Jun 28-Jun 14-Jul 27-Jul 2-Aug 8-Aug 16-Aug
IC + IT OOC
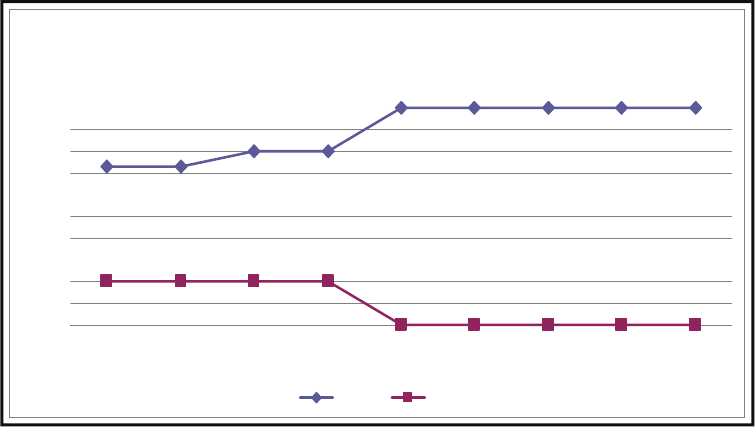
Transformational Leadership
Strategic Planning (3 EO)
57
Graph TL 3 EO – 5: CHF Measure
CHF Measure
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Baseline 2-Jun 14-Jun 28-Jun 14-Jul 27-Jul 2-Aug 8-Aug 16-Aug
IC + IT OOC
Transformational Leadership
Advocacy and Influence (4)
58
Advocacy and Influence
Source of Evidence 4
Describe and demonstrate the process(es) that enable the CNO to influence organization-
wide changes.
Marilyn Dubree transitioned from the Chief Nursing Officer to the Executive Chief
Nursing Officer (ECNO) in 2007. The organization had grown tremendously by virtue of the
addition of the Monroe Carell Junior Children’s Hospital, extraordinary growth in the outpatient
business and clinics, and the planned expansion of the University Hospital. The increase in the
size and complexity of the organization was diluting the role of the CNO simply due to the
diversity and demands one person had to attend to.
The executive leaders recognized the critical need to have Marilyn represent nursing at
the executive level. She was, and remains, well respected by the executive team. Marilyn
demonstrated that she was a valuable partner in the strategic decision making of the
organization and a driving force behind quality, patient, and employee satisfaction. Marilyn also
needed to be able to maintain the equal partnership of nursing with MD’s at the executive
level.
The executive leaders of the Medical Center actively supported and encouraged Marilyn
to restructure nursing leadership so she could fulfill the role and demands of the Chief
Executive Nurse. To that end, Marilyn transitioned to the Executive Chief Nurse and the added
Chief Nursing Officers for Vanderbilt University Hospital, Monroe Carell Junior Children’s
Hospital, the Vanderbilt Medical Group and the Vanderbilt Psychiatric Hospital.
The change positioned the role of the Chief Executive Nurse to partner with the Chief
Executive Officers in the clinical entities. The ECNO reports, as do the CEO’s of the clinical
entities to Dr. Wright Pinson, MBA, MD the Deputy Vice Chancellor for Health Affairs and the CE
of the Hospitals and Clinics. She is equally positioned to influence organizational change as are
the CEO’s.
Intentionally written into the job description of the ECNO are requirements to
participate in Executive teams and influence organizational change. The job summary (complete
job description provided in OO 2) states; “As a member of the VMC executive team, the CNO
supports and facilitates an interdisciplinary team approach to the delivery of care. This includes
creating a nursing environment in which collaboration is valued and excellence in clinical care,
Transformational Leadership
Advocacy and Influence (4)
59
education, and research is promoted and achieved. The CNO ensures the continued
advancement of the profession of Nursing at VMC.”
Key function number thee requires the ECNO to “participate in the planning,
implementation, and evaluation of clinical programs and services, assuring appropriate
resources for the delivery of care”. Key function four requires the ECNO to “Serve as the senior
spokesperson for Nursing, advising senior leadership of VMC and individual entities, institutes
and other affiliated institutions, (including the medical staff) by providing input about the
implications of decisions and change on the quality of patient care, on nursing practice, and on
nursing care providers.”
To enable Marilyn to influence organization wide change, the position of ECNO in
strategically placed on key committees within the structure. Table TL 4-1 describes the
organization wide teams where the ECNO is either an active participant or leader of the team.
Table TL 4- 1: Organization wide committees and forums where the Chief Executive Nurse is
an active participant
Committee Purpose
Clinical Enterprise
Executive Committee
The purpose of the Clinical
Enterprise Executive Committee is
to bring together leadership of
the Clinical Enterprise to address
strategic and operational topics
focused on PCC/Institute updates,
patient care operational issues,
and review of performance
alignment of common
infrastructure.
Influenced decision for VUMC
to be a tobacco free campus
which will be launched in
November, 2010
Administrative Affairs The purpose of Administrative
Affairs is to bring together key
clinical enterprise leadership and
medical center leadership to
address strategic and financial
topics focused on the clinical
enterprise.
Influences the agenda creation
for Leadership Assembly and
the alignment of such with the
strategic initiatives
With other Executives, defined
participants in executive and
leader incentive programs
Transformational Leadership
Advocacy and Influence (4)
60
Proposed and gained approval
for changes to NP
compensation
Medical Center Medical
Board
The broad, but not all-inclusive
purpose of the Medical Center
Medical Board is to represent and
act on behalf of the Medical Staff
while serving as the principal
committee to which all standing
and special committees report.
Influenced the decision to
support a policy allowing
families being present in
pediatric codes
Executive Committee of
the Medical Center
Medical Board
The purpose of the Executive
Committee is to affect a high
degree of communication
between the Medical Staff and
Medical Center administration
and to scrutinize and evaluate, on
a continuing basis, patient care in
terms of quality, convenience,
comfort and efficiency. It shall
make recommendations to the
Medical Center Medical Board
regarding the quality of overall
medical care rendered to patients
treated at the Medical Center.
Participates in decision related
to MD suspension
Quality and Safety
Steering Committee
Purpose is to align and
monitor contributions to the Pillar
Goals, manage projects and
improvement assignments, and
coordinate the readiness of
quality assurance, and regulatory
and accreditation improvement
Processes.
Approves quality plan and
quality goals.
Participated in decisions related
to the evolution of Medical
Director roles in quality
Quality and Safety Purpose is to guide and assist
executive leaders, the medical
Approves quality reports and
provides direction for quality

Transformational Leadership
Advocacy and Influence (4)
61
Council center board, and the board of
trust in fulfilling their
responsibility to oversee safety,
quality, and effectiveness of care.
initiatives
Information, Privacy
and Security Executive
Committee
The purpose of the Information,
Privacy and Security Executive
Committee is to regularly assess
the operating and computing
environment to identify risk
factors and define safeguards
against intentional or
unintentional disclosure of
Protected Health Information
(PHI), person-identifiable, or other
confidential or proprietary
information created, used, or
maintained by Vanderbilt.
Determines consequences for
individuals who breach
confidentiality
Determines use of social media
in clinical areas and on clinical
work stations.
Executive Faculty
Committee
Monthly meeting for the chairs of
all the SOM and SON to purpose is
to share information for the good
of the enterprise. Communication
and dialogue among the academic
leaders.
Provides updates regarding
clinical enterprise nursing issues
Clinical Enterprise
Group
“The purpose of CEG is to obtain
input, alignment, and ratification
of strategies with Department
Chairs and faculty on strategic
plans, capital plans, operating
budgets, public policy position
and other key items. This forum
also allows for information
sharing on various improvement
efforts in quality, services and
other areas. The financials are
Provides updates on the people
pillar performance and directs
clinical chairs on methods to
improve faculty performance
related to patient satisfaction
Transformational Leadership
Advocacy and Influence (4)
62
reviewed in detail monthly
identifying and discussing
variances based on budget.”
Human Resource Policy
Committee
The Human Resource Policy Sub-
committee is made up of
designated management
representatives from the major
areas of the University. Each
member of the committee is to
provide operational expertise on
how staff human resource policies
would impact their areas. The
role of this working committee is
to review recommended changes
to existing HR policies or to make
recommendations on the
development of new HR policies.
Once a policy reaches the
consensus of the members of the
policy sub-committee, the policy
is advanced to Policy Advisory
Board, comprised of senior level
executives or their designees for
review and approval.
Voting member that reviews
recruiting and hiring policy,
smoking, FLSA policiess (work
hours policy)
Clinic Redesign
Executive Committee
The purpose of the Clinic Redesign
Executive Committee is to support
and assist the clinics in designing
and implementing operational
models that improve access,
service, and evidence-based
delivery of quality healthcare
services for our patients. The
strategy is to: Redesign and
Approves nursing role changes
requiring evidenced based role
changes (triage nurses)
Transformational Leadership
Advocacy and Influence (4)
63
implement common/measurable
foundations for access operations
redesign and implement
common/measurable foundations
for clinical operations, and
support operations training and
development goals of VMG.
Organizational
Compensation
Committee
The purpose of the Organizational
Compensation Committee is to
address organizational concerns
about compensation and benefits.
Directs reviews for critical
nursing and other clinical roles
for market equity. Makes
recommendations related to
salary changes
[TL4-Exhibit A-1-CEEC Meeting Minutes Feb 2010, TL4-Exhibit A-2-CEEC Meeting Minutes Aug 2010, TL4-
Exhibit A-3-CEEC Nursing Presentation, TL4-Exhibit A-4-CEEC Nurse Residency Presentation] Other
minutes
are available upon request unless they are proprietary.
Table TL 4 – 2: Identifies the organization wide committees over which that Marilyn, as the
ECNO serves as the Executive Sponsor
Committee Purpose
Medical Center Staff
Advisory Committee
The purpose of the Medical Center
Staff Advisory Committee is to act
as an advisory group with both
administration and staff on
problems and policies that affect
the medical center and the people
it serves; to facilitate
communication between medical
center staff and administration on
all levels, including but not
necessarily limited to, Vanderbilt
University Hospital, Vanderbilt
University Medical School,
Vanderbilt University School of
Nursing, The Vanderbilt Clinic, and
Held retreat for group to create
charter purpose for this all staff
committee and how they need
to be effective in providdng and
receiving feedback. Employee
communitcation vehicle. Hold
quarterly meeting for chair and
executive te team.
Transformational Leadership
Advocacy and Influence (4)
64
medical center administration,
and to maintain effective
communication among staff
employees of Vanderbilt
University Medical Center.
Leadership Assembly The purpose of the Leadership
Assembly is for those medical
center leaders accountable for
pillar goal outcomes, to gather
quarterly with the Vice Chancellor
and other executive leadership.
These Leadership Assemblies
include the quarterly Elevate Pillar
Update as well as stimulating
leadership topics relevant to
sustaining a culture of excellence
and service.
Staff and Faculty
Satisfaction Survey
The purpose of the Staff/Faculty
(Community) Satisfaction Survey is
to utilize the tool drive employee
satisfaction and results across all
pillars organization-wide. The data
itself is shared with the staff and
actions are communicated based
on feedback.
Executive sponsor and thus
coordinates all work with the
vendor including contracting,
revisions to questions, action
plans and goals, time of
surveying
Patient Family Advisory
Council
The purpose of the Patient Family
Advisory Council is to offer
innovative ways for patients to
receive healthcare, become
healthy and stay healthy. This
council plans and evaluates
services, programs, policies, and
teaching materials.
Executive Sponsor attending
monthly meeting sharing and
hearing feedback. Work
influenced position on tobacco
free campus, patient education
work
Transformational Leadership
Advocacy and Influence (4 EO)
65
Advocacy and Influence
Source of Evidence 4 EO
Describe and demonstrate one (1) CNO-influenced organization-wide change.
Purpose/Background
VandyWorks
The Staffing Task Force was formed in 2001 as a request of the Chief Nursing Officer,
Marilyn Dubree, MSN, RN, NE-BC, to ensure that Vanderbilt Hospital and Clinics have the
appropriate staff resources properly deployed to provide consistent, safe, quality care. Through
the work of this group, it was determined that an electronic tool was required to achieve this
goal. A return on investment (ROI) was completed to quantify organizational benefit of an
automated tool.
The Staffing Task Force surveyed VUMC nurses to understand their unique staffing
requirements. Over an 18 month period, 13 vendors were evaluated to find the best product to
achieve our organizational goals. Workbrain (VandyWorks) was chosen as the best match due
to their track record of innovation and flexibility in retail and transportation markets.
Workbrain was willing to partner to develop a unique healthcare solution that goes beyond
basic staffing and scheduling and incorporates quality, safety and the ability to expand.
The initial cost of the Workbrain program outlay was $300,000. Ongoing support of the
project was an additional cost of the project. Functional and technical teams were created to
continue implementation and support of the work. Marilyn Dubree, MSN, RN, NE-BC, CNO,
advocated for the capital dollars and ongoing operating budget to support this project. (More
information is provided about VandyWorks in EP 8, 9, 11 & 12)
CATS
As the Medical Center continued to grow, Marilyn Dubree, CNO, helped to lobby for a
better way to monitor the nursing staff licensure, certification, education and experience.
Prior to an electronic system, each unit kept paper records to track the information on their
staff. The process was not consistent and it was challenging to have information readily
available during surveys by the state and JCAHO. Nursing leadership partnered with Human
Resources to make suggestions on the design of a program to fill this need. Marilyn presented
the proposal for the required capital outlay and ongoing operating budget to the board and
received approval.
Transformational Leadership
Advocacy and Influence (4 EO)
66
The Credentials Application Tracking System (CATS) was initially created to track nursing
licensure and certifications in 2005. Vanderbilt Medical Center identified that a single tracking
tool would be optimal so that a repository of information would be available for collecting data
on certification and licensure for nursing. A single tool would assist in monitoring license and
certification compliance for all staff as well as store years of experience used for salary equity
reviews among our current employees. Prior to CATS there was a gap in the system as this
information was not stored in any electronic or useable format.
Vanderbilt partnered with Infoworks, the computer software company used to write an
electronic evaluation program for Vanderbilt that is still in use (VPES). Infoworks was asked to
write a program to track licensure and certification for our professional nursing staff. The initial
cost of CATS was $60.00. In 2006 nursing was the primary user. In 2008, pharmacy technicians
were added. In 2009 licensure for Rehabilitation (PT/OT), Respiratory Therapist, Radiology
Technologists, Pharmacists, Laboratory Technologists, and Dietary/ Nutrition were added. In
2010, anesthesia technicians were added. In addition, all entry level positions in patient care
support, service support, and nutritional support were added. Case managers and Utilization
Management were also added to round out the clinical enterprise. The total cost of CATS to
date has been approximately $230.000 for the programming plus the additional support
supplied by HR to manage the program.
Methods/Approach:
VandyWorks
The Staffing Task Force (now Clinical Workforce Committee), under the direction of
Marilyn Dubree, MSN, RN, NE-BC, CNO, worked with Human Resource to write a clinical policy
on the “Schedule Process” for all the Medical Center staff. The policy included schedule length,
maximum hours of work and gave general parameters for vacation, holiday and personal day
scheduling that should be used for areas to write their own unit specific policies. (Reference
policy Patient Care Services: Scheduling Process, CL 20-06.25 – provided in EP 9) These unit
specific policies are reviewed by the Clinical Workforce Committee to ensure they were
consistent with the clinical operation policy.
Initially VandyWorks was piloted in two units 9N and 9S. The manager, assistant
managers, charge nurses and staff were given extensive training on how to use the program.
There were many focus session groups to gain knowledge on how the system needed to work
and how to make the work of the charge nurse easier to manage staffing. Using this pilot
information, the rollout process was planned. The VandyWorks team would meet with each
area and give a demonstration and discuss the setup process. The staff on the units were
involved in the process from the beginning and offered feedback. Unit specific rules were in
Transformational Leadership
Advocacy and Influence (4 EO)
67
place to provide consistency, fairness, and safe staffing decisions. Ongoing training was given
as new capability is added to the system. The team now has a full time RN educator who is able
to provide a clinical focus to the work.
After the implementation of the system in in-patient areas in both the adult and
pediatric hospitals, the focus has changed to meet the needs of the outpatient and procedural
areas. This work is ongoing. For some out-patient areas the VandyWorks system has not
matched the unique staffing requirements and partial shift times. These areas are brought on
line to use the request off function that allows tracking of leaves and to receive alerts for
certification and licensure via the CATS information.
CATS
When every staff member is hired, our HR tracking system, PeopleSoft automatically
loads their hiring information into CATS (unit, job code, etc). This is done by department
numbers. Then licensure, certification, education and years of experience are gathered by their
department and entered into CATS. This data follows the employee throughout their
employment at Vanderbilt even thought they may change positions. When staffs transfer to
new areas, PeopleSoft automatically makes those changes.
The department administrator (PAF responsible) and the department manager have
assigned access to CATS based on their job role in the People Soft system. Either of these two
responsible persons can delegate up to two department assistants per area to help assist in
data entry. The department manager has the overall responsibility of keeping this data up to
date in the system.
Licensure and other information can be updated as needed (expiration times).
Managers are also required to check the data annually at evaluation time. CATS is interfaced
with VPES which is our electronic evaluation system. When a manager is doing the staff
evaluation, an automatic notification comes up about reviewing CATS. The manager is then
linked directly into that staff member’s CATS database to be able to review their information.
All staff also have a “read only” capability for their CATS information. The system is set-up in
such a way that no one (manager, supervisor, etc.) can change or update their own
information, their one-up must do that. That is one of the many safe guards of the system.
New capabilities added this year include a date stamp for primary source verification
(State Website) and pop up messaging to remind managers or designees to enter additional
information related to certification and licensure for Advanced Practice Nurses and Emergency
Medical Personnel. The changes will improve complete documentation in the system.
Transformational Leadership
Advocacy and Influence (4 EO)
68
The system uses a stop light monitoring system:
Green- information is current
Yellow- information will expire at the end of the current month
Red- information has expired and needs updated
This allows the manager or designees to see at a glance when staff information needs updates.
In addition, managers of the various areas can run reports for their specific units from
any information located in CATS. They can do years of experience, licensure expirations,
certification expirations, and many others. This provides a unique flexibility to the managers.
CATS administrators have the flexibility of adding additional licenses and certification
when needed. This flexibility in the programming has allowed Vanderbilt the ability to manage
the information required as new areas/departments have been added to the system over time.
Evaluation/ Outcomes:
VandyWorks
VandyWorks is used for reporting and tracking productive and non-productive hours (in-
services, sick, vacation, FMLA, etc). It is also able to track staff that clock in early for their shifts
or out late when leaving. Bi-weekly rollup reports are sent to the administrative leaders
showing hours and dollars associated with these costs so that the managers can manage these
hours to a minimum. Managers can run drill down reports that specifically identify staff that
are on the reports. Working to reduce the “in early” hours are a direct cost savings to the
Medical Center by managing incidental overtime. Managing these hours along with reducing
the hours needed to create and maintain a schedule for the units has been the ROI needed for
this project.
Staff satisfaction with the system has been positive. They are able to access their
schedule, make time off or swap shift requests from any computer. Feedback supports that it
makes the schedule process fair and allows easy access. Feedback indicates there is a high
learning curve but after the learning curve the system is user friendly and provides them with
the information they need.
The VandyWorks technical team has been able to add new alerts to the system by
pulling data from CATS in relation to nurse licensure. One example is nurse licensure compact
information. The system can look at the employee’s address and send an alert message when
the state of residency does not match the license entered into the system. This alert
information is validated monthly to ensure that staff licensure is correct to meet compact
Transformational Leadership
Advocacy and Influence (4 EO)
69
requirements. When staffs are identified, the unit/department manager is notified to follow up
for compliance and update the system or note approved variance from the rules written for the
VandyWorks system.
CATS
The CATS database has the ability to send the license and certification information to
the VandyWorks program, allowing for reminders of upcoming expirations for staff and their
leaders. For licensed staff using the VandyWorks system, if their license has expired in the CATS
system they are unable to be scheduled until this is updated. Recent updates in VandyWorks
can also project out for scheduling six weeks in advance and color code staff who have a license
that will expire in the future.
The CATS team partnered with the Resuscitation Department which provides
certification for VUMC staff for BLS, ACLS, PALS, etc. They now enter the new certification
expiration dates into the CATS system for each all Vanderbilt staff members attending. This
gives very accurate records for these certifications in the system. It has allowed the team to
run reports and identify how many staff members have expiring certifications and will need
training. This data allows the Resuscitation Department to more accurately plan on the number
of classes needed for each of the certifications required.
The CATS system has also been able to communicate with the Vanderbilt Performance
Evaluation System (VPES). Through this communication information is available during the
evaluations related to the employee’s status of required licensure and certification. RN
licensure and BLS information is uploaded from the CATS data. The CATS system integration
into VPES allows managers to easily and efficiently complete primary source verification for
licensure at the time of the annual evaluation.
The years of experience data in CATS is used by HR to determine salary for current staff
comparison. Using regression analysis, HR can determine cost when implementing market
adjustments with this data. This has been a significant improvement and time saver over prior
years saving time and dollars.
The CATS database has been invaluable during state and JCAHO visits. Reports are
easily pulled that detail all licensed personnel, type of licenses and tracking of expiration dates.
The system can also be used to track all required certifications for the different professions.
Each unit/department has designated staff that can access and maintain each group’s data for
their staff and run reports.
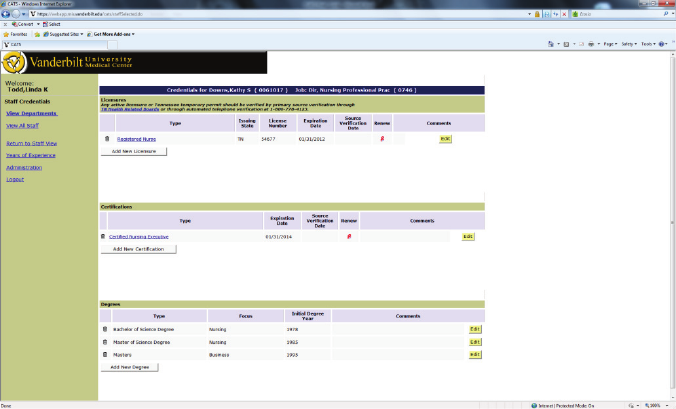
Transformational Leadership
Advocacy and Influence (4 EO)
70
Summary
Marilyn Dubree’s ability to actualize her vision of automated systems for scheduling and
tracking of required human resource licensure and other compliance data for nursing has had
far reaching and positive effects on the organization. The systems designed for nursing are now
used throughout the organization. The human resource transaction systems are now
organization wide and allow the organization to:
Accurately and efficiently track licensure and competency status for individual staff
Ensure required licensure and certification through automated reminders for staff and
managers
Improve efficiency of verification of licensure requirements
Use years of experience data for equity reviews for the implementation of market and
other organization wide adjustments as well as for individual reviews
Improve the ability of staff to participate in creating work life balance by participating in
the scheduling process
Examine human resource utilization to improve efficiency (example: timeout report)
[TL4EO-Exhibit A-1-VandyWorks Advisory Minutes Sept 10, TL4EO-Exhibit A-2-VW Project Team
Minutes Sept 2010, TL4EO-Exhibit A-3-News You Can Use Sept 2010, TL4EO-Exhibit A-4-
VandyWorks Alert]
Graph TL 4 EO – 1: CATS Screenshot

Transformational Leadership
Advocacy and Influence (4 EO)
71
“In their own words”
Salary and Compensation Comparisons From Human Resources
“Prior to CATS, the HR Office of Compensation had attempted several methods for
determining salary, with limited success, if an RN had x number of years of experience for
current staff and new hires. Our goal was to use the full pay range for individuals in the RN title
considering their years of nursing experience and their last performance evaluation score across
the organization, not just within a specific unit. Any attempt at data collection was via an Excel
Spreadsheet requiring a manual update each time the data was requested as well as the
logistical challenges of obtaining this information from each unit across the Clinical Enterprise.
When determining new hire salary rates, Recruitment did not have up-to-date information for
comparing against similar individuals within the organization beyond the unit level resulting in
inconsistent salary offers and creating bidding wars among hiring managers for the same
applicant. And, Compensation could not easily determine a cost estimate for a nursing market
adjustment.
With the creation of CATS, we now have a mechanism for capturing years of experience
that have greatly improved our processes. Years of experience data in CATS updates
automatically so that once the data is entered, it automatically adds the years without requiring
any additional work from the manager. We have the ability to pull RN data for the entire
Clinical Enterprise to compare individuals across entities and units with the same years of
experience and performance evaluation scores. Data is provided to Recruitment so that salaries
can be determined for new hires without disrupting salary equity with current staff, and reduces
bidding wars among hiring officials from different departments. Compensation has used the
data from CATS to conduct organizational wide salary equity reviews, and cost projections for
market adjustments. This process is invaluable for cost projections of widespread populations
such as nursing or entry level staff, each group with 2500+ employees. This method of reviewing
salaries for nurses has also been applied to Pharmacy Technicians, Rehab, Respiratory,
Radiology, Labs, and Dietitians. Information is power, and we have provided this invaluable
data and system to our managers, recruiters and compensation teams for evaluation and use of
efficient and effective methods to perform daily functions of their job.”
Leslee Hughes, MA, PHR, Manager, Compensation Human Resources
“The ability of VandyWorks and CATS to communicate is a huge win. Prior to this, the educator
or assistant manager manually tracked pending expirations and emailed staff. With this current
capability, the manager, administrative assistant and staff member receive an email beginning
90 days prior to expirations allowing plenty of opportunity for scheduling and completion of the
needed task. In addition, the nurse is automatically removed from the schedule in VandyWorks
if they fail to renew their nursing license prior to the expiration date.”
Debbie Shinkle, RN, BSN, MHA, M Ed, Manager, VCH 6A/B, Pediatric Hematology & Oncology

Transformational Leadership
Advocacy and Influence (4 EO)
72
“Having CATS and VandyWorks interfaced is helpful with automatic notices about license
expiration. This interface is also helpful with alerting staff about pending certification
expirations (BLS or ACLS). It gives a 90 day and 30 day alert.”
Julie Foss, MSN, RN, NE-BC, Manager, MICU VUH
“The reports allow us to track prior to expiration dates and provide staff with ample time to
renew their license and certification to meet their job requirements. Having staff removed if
their license is expired helps as a last and final warning to both the manager and the staff
member.”
Richard Corcoran, BSN, MSHA, RN, Manager, 9 North, Surgical Step down, VUH
“CATS has been valuable to the pharmacy to help us maintain updated information on licensure
status of our staff. The notification features are a great motivator to our staff to process
needed paperwork in situations where renewals may not be as timely as desired.”
Mark Sullivan, PharmD, Director, VUH Pharmacy
“The CATS database has provided us in the Respiratory Care Department with several
advantages:
1. We are now able to easily generate a custom report with all of our staff’s licenses,
expiration dates and special endorsements. This has been very helpful specifically when
we had our recent TN State Department of Health inspection and they requested a list of
all RTs, with license numbers, expirations dates and ABG endorsements. It only took a
minute to generate this from the CATS database.
2. The CATS database provides us with a quick visual of the status of all our staff with
regard to special certifications, i.e. Fundamentals of Critical Care Support (FCCS), ACLS,
PALS, BCLS training.
3. The CATS database also assists us with tracking years of experience so we can be
assured we are maintaining pay equity with all of our staff.
Anna Ambrose, RRT, MHA, Administrative Director, Respiratory Care VUH
“CATS have been helpful to me in tracking the renewals. One less spreadsheet I have to keep. It
automatically emails employees reminding them of their expiration date. One less email I have
to send. I can then update the system when they have renewed their license.”
Cindy Johnson, Pharmacy

Transformational Leadership
Advocacy and Influence (4 EO)
73
“It has been helpful to me in tracking renewals and reminding staff by the automatic emails. It
is very helpful!”
Rhonda Tully, CRA, MBA, Administrative Director, Department of Radiology
Transformational Leadership
Advocacy and Influence (5)
74
Advocacy and Influence
Source of Evidence 5
Describe and demonstrate how nurse leaders guide the transition during periods of planned
or unplanned change.
Vanderbilt is a system that has as one hallmark, the ability to plan and execute on
change. The drive to constantly improve, innovate and lead in patient care delivery
effectiveness and efficiency creates a culture where change is expected. The environment
attracts those who find change intellectually and professionally rewarding. Whether change is
“top down” or initiated from staff, nursing leadership is always at the heart of the change
planning, implementation and evaluation processes.
The Shared Governance model at Vanderbilt provides a strong structure to engage all
levels of nursing in the change opportunity. The structured described in OO 11 and SE 1, is our
vehicle for shared decision making, provision of feedback, and evaluation of change
effectiveness. Leaders use the rich dialogue of shared governance collaborative teams and
structures at all levels to recognize the need for change, test change ideas, to refine plans for
change, implement and evaluate change.
As change ideas emerge, the Nursing Executive Board places the change ideas against
the strategic direction for nursing, testing the congruency with over arching objectives. The
Nursing Administrative Boards which are both organization wide and entity specific are the
vehicle for accountability of clearly planning change across the organization. Nursing Leadership
Boards implement changes and use their area and Units Boards for rapid cycle improvement,
evaluation and feedback of real and proposed change.
Nursing leaders participate in enterprise wide committees and help those teams pace
the rate of change as nursing seems to be the common denominator impacted by all
organizational change. The collaborative nature of nursing with all disciplines positions nursing
leaders to be involved in designing change throughout the organization.
Three examples of how nursing leaders manage planned and unplanned change are described
below.
Transformational Leadership
Advocacy and Influence (5)
75
Critical Care Nurse Practitioner Program
Purpose/Background
Patient volumes have been on a steady increase at VUMC. The strategic plan for the
organization included the addition of a new Critical Care Tower with 3 critical care units
opening in November of 2009. These units would accommodate increases in the Surgical
Intensive Care Unit (SICU), Medical Intensive Care Unit (MICU) and Neuro Intensive Care Unit
(NICU). As planning occurred for these expanded units, it was recognized that additional nurses
in advanced practice roles would be need to provide comprehensive, team based critical care to
the increased patient populations. This need was further reinforced by the unplanned reduction
of resident hours due to training program restrictions.
Pam Jones MSN, RN, the Chief Nursing Officer for VUH, was the executive leader for this
project. Other team members included Dr. Lee Parmley (Executive Medical Director for Critical
Care), Dr. Allen Kaiser (Chief of Staff – VUH), Clare Thomson-Smith, RN, APN, JD (Director,
Center for Advanced Practice Nursing and Allied Health), Devin Carr, RN, MSN (Administrative
Director) and Deeanne Moore (APN – NICU).
The need for a systematic plan and approach to this was identified as a goal for the CNO
during the annual goal setting process in July of 2008. A multidisciplinary group of leaders was
put together to assess this need and develop a standardized model. A roadmap for decision
making was developed and presented to the CEO on 8/25/2008. [TL5-Exhibit A-1-ICU APN
Coverage Plan Development]
The project team conducted a site visit to Duke University Medical Center which had
been identified as a best practice site for the use of advanced practice nurses in critical care.
Clare Thomson-Smith, Director for the Center for Advanced Practice Nursing and Allied Health,
also conducted telephone interviews with other experts in the utilization of advanced practice
nurses to assess best practice.
A model was developed in collaboration with the ICU Medical Directors and other
appropriate faculty members and presented to administration for approval. [TL5-Exhibit A-2-
ICU APN Critical Care Model] This model included the addition of advanced practice nurses at a
ratio of one (1) APN to eight (8) patients. The numbers of APNs hired allocated per unit varied
depending on the resident coverage. The appropriate number of APNs were placed in the
budget and hired in a staggered manner in preparation for the opening of the Critical Care
Transformational Leadership
Advocacy and Influence (5)
76
Tower. The staffing compliment was determined and put into the budget for the fiscal year,
2009-2010 which began on July 1, 2009.
In addition to the model development, the physician leaders of MICU developed an
extensive training program to ensure competency for the MICU APNs. Historically, the MICU
did not utilize APNs at all and Dr. Art Wheeler, Medical Director of the MICU, embraced the
concept with academic enthusiasm. The curriculum is attached. [TL5-Exhibit A-3-MICU NP Core
Curriculum]
Meal Break Time Keeping Unplanned Change
In November, 2009, Vanderbilt University Medical Center attorneys were notified of a
class action lawsuit that had been filed against Vanderbilt by a former nurse. The nurse alleged
that Vanderbilt had not compensated her and other of Vanderbilt employees for missed meal
breaks. We learned this was a common occurrence that was happening throughout the
country.
The situation was that the time and attendance system at Vanderbilt (Kronos) was
programmed to deduct 30 minutes from the total time an employee was clocked into work as
an automatic deduction for a meal break. If an employee missed the meal break, the employee
should self-correct by cancelling the meal break deduction or reporting the missed meal break.
Reporting the missed break allows the time-keeper to cancel the deduction. The lawsuit
alleged that employees who did not get a meal break due to work responsibilities were not
always compensated for that time. The lawsuit was based on the Federal Labor Standards Act,
which requires that employees be paid for all hours worked, including meal breaks missed by
employees or meal breaks that were interrupted in such a way that the employees were not
able to fully enjoy their meal breaks.
The person involved in the lawsuit was the Executive Nursing Officer and became the
Executive leader responsible for managing the situation. Since the allegations in the lawsuit also
related to non-nurses, David Posch, the CEO of the Vanderbilt Medical Group, became Marilyn
Dubree’s Executive partner.
The actions taken to resolve the matter included:
Increase all supervisor , manager and leader understanding of and ability to comply
with the federal regulations and Vanderbilt University Policies on meal breaks
Transformational Leadership
Advocacy and Influence (5)
77
Correct any error that had occurred in compensation
Clarify the rationale for the automatic meal break deduction in the time and attendance
system
Reinforce the expectation that all staff take regular breaks
Maintain a process of time keeping that is efficient and effective for staff and the
organization
An Executive Committee was formed to manage this situation with far reaching
implications to the organization. The Committee included:
Marilyn Dubree, RN, MSN, NE-BC, Executive Chief Nursing Officer
David Posch, MS, CEO Vanderbilt Clinic and Executive Director Vanderbilt Medical Group
Lynn Webb, PhD, Assistant Vice Chancellor for Health Affairs
John Manning, Assoc. VC for Health Affairs and Chief Admin Officer and Sr. Associate
Dean for Operations and Admin, SOM
Wright Pinson, Deputy Vice Chancellor for Health Affairs and CEO of the Hospitals and
Clinics
An Education and Communication Committee was also formed and included:
Susan Mezger, CCP, SPHR, Director, Human Resources
Terri Minnen, Senior Consultant, M.Ed.
Pam Brown, Director, Organizational Effectiveness Team
Debora Shiflett, Director, VUMC Financial Training
Karen Anne Rye, Assistant Director, Enterprise Wide Functions
Debianne Peterman, Ph.D., MSN, RNC-NIC, NE-BC, Director, NE & PD
John Callison, Senior Deputy General Counsel
Transformational Leadership
Advocacy and Influence (5)
78
James Floyd, Associate General Counsel
Veronica Burns, Senior Director, Human Resources
Nannette Vaughan, Manager, Department of Employee Relations
Payroll office and Management Information Systems
Action Steps
The first action was to review the Vanderbilt policies and understand if the policies were
consistent with Federal requirements. The policies were reviewed and, while the policies were
consistent, some revisions were made to clarify any ambiguities.
The second step was to investigate if Vanderbilt was following the stated policies. To
that end, hundreds of supervisors, managers and timekeepers were interviewed to assess their
practices related to time keeping and meal breaks. This was accomplished with the assistance
of external legal manpower. The assessments found that there was variation in the
administration of time keeping related to time and attendance. At this point, Vanderbilt
recognized that there was potential for error in payment to employees and began to action
plan.
Based on the principle for doing the right thing for employees, planning was focused on
communication, education, and identifying error in payment. A team of human resource,
training and financial experts was assembled to take the next steps. A process was designed to
inventory the number of staff who might not have been paid accurately. The process that was
developed was a survey methodology.
The survey was developed with the intent that it would be made available to all current
and former staff using the Kronos system for time keeping in the last two years. The survey was
developed to provide each staff member the following employee-specific information: total
number of meal breaks that were deducted from their pay for the previous two years and the
number of meal breaks that were credited back (logged as “no meal break”) in the Kronos
system. With that information, staff members were asked to declare the number of meal
breaks they missed and were not compensated for in the two year period. [TL5-Exhibit B-1-Staff
Training]
Vanderbilt’s intention was to do the right thing for employees trusting in the honesty of
employees to self-report accurately. As a result of Vanderbilt’s program of education and self-

Transformational Leadership
Advocacy and Influence (5)
79
correction (including voluntarily paying staff for all reported meal breaks missed); the lawsuit
was dismissed at an early stage.
Communication and education for this entire effort was daunting. A detailed training
plan is provided for review. [TL5-Exhibit B-2-Training and Communication Plan]
Training/Education
Managers and supervisors were first trained in required sessions. [TL5-Exhibit B-3-
Manager Training]
The objectives of the supervisor training were to:
Define the supervisor’s responsibility and accountability for:
o Reconciling and approving payroll data
o Overseeing the timekeeping function
o Monitoring of trends and practices within department
o Communication process of policy and procedures to staff
Identify the correct procedure for reviewing and approving time records when a staff
member has not been able to take an uninterrupted meal break during work hours.
List examples of best practice to create an environment where staffs routinely take an
uninterrupted meal break.
After leaders were trained and aware of the plan, the training effort turned to staff. There
were multiple sessions at various times in order to provide sessions for those working different
shifts.
The training objectives were to:
Define an “uninterrupted meal break.”
Identify the correct processes to follow to cancel an automatic meal deduction in
Kronos.
Transformational Leadership
Advocacy and Influence (5)
80
List the steps required to ensure that the Kronos time record is accurate.
Once the training was complete, staff began taking the survey. Vanderbilt provided a
helpline for those needing assistance with their survey information. In addition, staff was able
to go to dedicated computer rooms during the survey period in case they did not have easy
access to a computer nor needed additional assistance. After the survey was closed, it was
recognized that some staff who did not participate in the survey wanted to be included. The
survey was reopened to staff who had not taken the survey initially.
Once staff had declared the meal breaks for which they believed they should be paid,
letters were written to staff with an explanation of the compensation they would receive. They
were paid the average rate of pay for the two year period for the hours they reported as not
paid.
A helpline and frequently asked questions website were developed for ongoing support
to staff, supervisors, managers and leaders. The Executive Leadership team continues to meet
once a week with additional meetings at least twice a month to monitor progress of the effort.
Summary
This entire event caused Vanderbilt to learn about an opportunity for improvement. The
event created recognition of the need for ongoing and predictable education related to time
keeping. In addition, it created a model for managing meal breaks that is now being extended
to other employees who do not use the Kronos system. The event tested the organization’s
ability. Never before had such an extensive institution-wide education effort been executed in
such a short time frame. Perhaps, most importantly, the event tested Vanderbilt’s commitment
to employees and for defining the “right thing to do” approach to providing fair treatment to its
most precious resource - Vanderbilt staff.
Measureable outcomes include:
Policy was revised (provided for review)
Hundreds of managers, supervisors and timekeepers interviewed
Approximately 1,600 managers, supervisors, administrators were trained
Transformational Leadership
Advocacy and Influence (5)
81
Approximately 10,000 employees using Kronos were trained (40 sessions which
provided 24,700 available seats)
7217 employees responded to the survey
2,782employees were compensated for missed meal breaks
VUMC H1N1 Pandemic Response
When the outbreak of H1N1 began in April 2009, through an interdisciplinary approach
VUMC was ready to respond. On the weekend of the initial outbreak the Chief Medical Officer
& Associate Vice Chancellor for Clinical Affairs, Chief Hospital Epidemiologist, and VUMC
Emergency Preparedness Coordinator kept in close contact by phone on the developing health
emergency. On Sunday, April 26
th
, the decision was made by this group to have an Executive
Briefing early Monday morning due to the extent of the developing H1N1 outbreak. The VUMC
Emergency Preparedness Coordinator , Pam Hoffner, RN, MSN was also in contact with the
Regional Hospital Coordinator and requested a TN Department of Health (TDH) Hospital
Advisory Committee conference call on Monday to ensure all TN hospitals were updated on the
situation, communication lines were established, and to ensure a well coordinated response to
the health emergency.
At the first Executive Briefing, it was decided a gap analysis of the VUMC Contagious
Pathogen Plan needed to be completed to ensure readiness for a bio health emergency
response. A Vanderbilt University representative would be included in all executive level
meetings to ensure the University response plan was in place. There were a series of daily
Executive Briefings and Operational meetings over the next several days which where chaired
by Executive Nursing Leaders in collaboration with the VUMC Emergency Preparedness
Coordinator, and Executive and Senior Medical Leadership. The VUMV Emergency
Preparedness Coordinator and Director of Infection Control attended frequent TDH conference
calls and conference calls with the Regional Hospital Coordinator.
The Monroe Carell Junior Children’s Hospital at Vanderbilt received their first suspected
H1N1 Influenza patient. With the arrival of the first patient, the decision was made to increase
surveillance activity to include virtually all ports of entry into the Medical Center. A partial
activation of the Emergency Operations Center (EOC) allowed for a succinct interdisciplinary
response to the health emergency. Executive briefings were conducted on a daily basis.
Transformational Leadership
Advocacy and Influence (5)
82
The Contagious Pathogen Plan gap analysis performed by the VUMC Emergency
Preparedness Coordinator in collaboration with the Executive Chief Nursing Officer revealed
gaps in HR, Triage, Surge Capacity, Education, Vaccine and Antiviral Allocation/Distribution, and
Ethics. To remedy these areas of vulnerability, six interdisciplinary pandemic planning teams
were formed to address each gap. A chair (from senior leadership) was assigned to each team
and the majority of team meetings were facilitated by the VUMC Emergency Preparedness
Coordinator. The teams were given a series of tasks to rectify the gaps and these were to be
completed within a designated time frame set by the Chief Medical Officer & Associate Vice
Chancellor for Clinical Affairs.
The partially activated EOC remained operational along with the daily Executive
Briefings for a total of nine days at which time H1N1 Influenza activity in the state of TN
stabilized. During this time, it became apparent there was a need for a medical director to be
assigned to the Department of Emergency and an appointment was made by the Chief Medical
Officer & Associate Vice Chancellor for Clinical Affairs.
The need for a Pandemic Tabletop Exercise for Executive and Senior Medical Leadership
to test the newly revised Contagious Pathogen was entertained by the VUMC Emergency
Preparedness Coordinator and Executive and Senior Medical Leadership agreed this would be
an excellent educational method to utilize to train senior leadership about pandemic planning.
A decision was then made to hold the exercise in early September.
During the months of May, June, July, and August the Pandemic Planning Teams
continued their work until their task lists were completed. Periodic updates were given to
Executive Leadership by the VUMC Emergency Preparedness Coordinator and the newly
appointed Medical Director for the Department of Emergency Preparedness.
The increased surveillance efforts continued at VUMC throughout the summer months
and H1N1 Influenza was elevated to a pandemic by the World Health Organization (WHO) in
the month of June. During the months of July and early August the VUMC Emergency
Preparedness Coordinator served as a liaison and consultant to Vanderbilt University in their
pandemic planning efforts with their start-up of the fall semester. She also assisted the
Director of Student Health, Dr. Hanson, in obtaining a Memorandum of Understanding (MOU)
with CVS pharmacy in an effort to streamline the filling of antiviral prescriptions in order to
streamline patient throughput in the Student Health Clinic.
The Labor Day weekend proved to be the start of the second wave of the H1N1
Pandemic for Children’s Hospital. It hit with a vengeance that allowed us to test our plan. This
Transformational Leadership
Advocacy and Influence (5)
83
was followed by an outbreak on the VU campus side. The other metro hospitals didn’t
experience a large second wave of H1N1 like VUMC.
A multidisciplined H1N1 Steering Committee comprised of senior leadership was formed
at the request of the VUMC Emergency Preparedness Coordinator to establish a mechanism to
handle the second wave of the pandemic. This proved to be a good forum to coordinate the
second wave response efforts and minimally disrupted hospital operations. A weekly
conference call was also conducted with the University side and was attended by the VUMC
Emergency Preparedness Coordinator.
In early September an H1N1 Pandemic Exercise was conducted and attended by 106
faculty and staff members who included a large portion Executive and Senior Medical
Leadership along with VU Executive Leadership and key Medical Center departments. The main
objective of the exercise was to educate senior leaders and key departments about the newly
revised Contagious Pathogen Plan and the pandemic planning process. This exercise was
planned and facilitated by the VUMC Emergency Preparedness Coordinator.
Following the exercise, the VUMC Emergency Preparedness Coordinator was utilized as
a consultant for pandemic preparedness initiatives in several medical center departments and
divisions. Faculty and staff were also assigned to a mandatory online inservice on the VUMC
Contagious Pathogen Plan and Pandemic Planning. The VUMC Emergency Preparedness
Coordinator was an active participant in the development of this inservice in collaboration with
the pandemic planning education team, infection control, and the Chief Hospital
Epidemiologist.
During the fall and winter months, the adult side of VUMC experienced a few surges in
H1N1 influenza cases that primarily affected the MICU. The H1N1 Steering Committee and VU
conference calls continued to meet on a weekly basis and H1N1 issues were addressed on a
weekly basis in this forum some of which included: weekly surveillance reports on flu activity
and N-95 mask usage, antiviral distribution, H1N1 vaccination distribution, education of
patients and visitors, and ECMO issues. At the beginning of December H1N1 surveillance
reports indicated a marked decrease in disease activity in TN and at VUMC. At this time a
decision was made by the H1N1 Steering Committee members to decrease meeting frequency
to bi-weekly. In early January, the flu surveillance systems continued to indicate very little
H1N1 activity and the decision was made to discontinue the H1N1 Steering Committee with the
understanding to resume the meetings if activity started to increase.
Transformational Leadership
Advocacy and Influence (5)
84
At this time the VUMC Emergency Preparedness Coordinator continues to monitor
H1N1 activity in collaboration with Infection Control and the Chief Hospital Epidemiologist and
the pandemic planning process continues at the medical center.
In summary, the success of VUMC’s and Vanderbilt University’s response plans was
due, in large part, to a exceptional degree of interdisciplinary collaboration within Vanderbilt as
well as extensive external communication and collaboration at the local, state and national
levels.
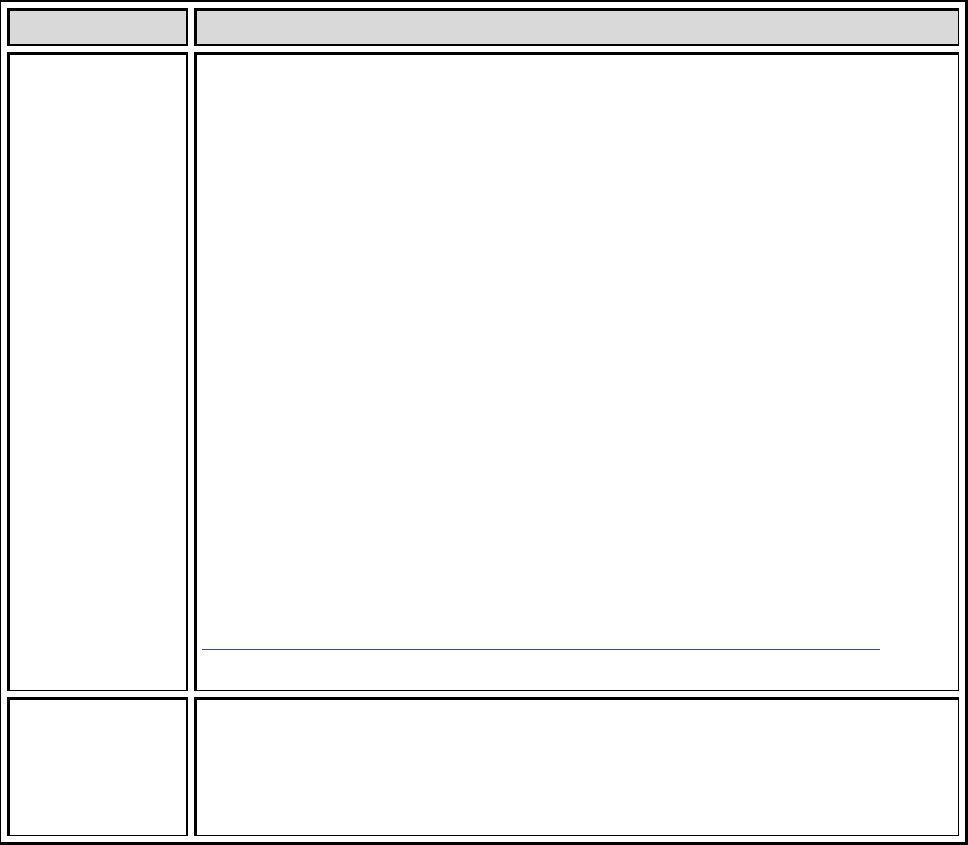
Transformational Leadership
Advocacy and Influence (7)
85
Advocacy and Influence
Source of Evidence 7
Describe and demonstrate how nurse leaders value, encourage, recognize/reward, and
implement innovation.
Examples and methods of valuing, encouraging, recognizing and rewarding innovation
are found across the organization. The following are some of those examples.
Table TL 7 – 1: Examples
Recognition and
reward through
the Center for
Frontline
Leadership.
Through the Center for Front Line Leadership program, Vanderbilt Nursing
invests in training aspiring leaders into the field. Since 2006, Vanderbilt has
partnered with the Advisory Board to make the Center for Frontline Nursing
Leadership program available to Vanderbilt nurses.At the end of the
program, all participants are honored by presentation of their projects to
the Nursing Administrative Baird members. [TL7-Exhibit A-1-CFNL
Graduation Jan 2010]
The Future of Nursing Leadership Award was initiated in 2007 to recognize
the incredible impact of frontline nurses who have completed the Advisory
Board Academies’ Center for Frontline Nursing Leadership. Tanika Wilson,
RN, BSN, Assistant Manager PCCU was recognized for her work on “Drip
Double Check reduced medication Errors” in 2009. Debra Grimes, RN,
Charge Nurse in Women’s Health was recognized for her work in “Creating
an Acuity Based Staffing Model” in 2008. Both of these award winners are
highlighted on the Vanderbilt Nursing Web site. The web site provides
videos of each of these award winners.
http://www.mc.vanderbilt.edu/root/vumc.php?site=vanderbiltnursing&doc=18887
Annual Nursing
Awards
Every year nurses from across the VUMC system nominate the best and the
brightest for recognition at Vanderbilt. The nurses to be awarded are
selected by a committee. The nominees and the award winners are
recognized annually at a presentation ceremony during Nurses week.
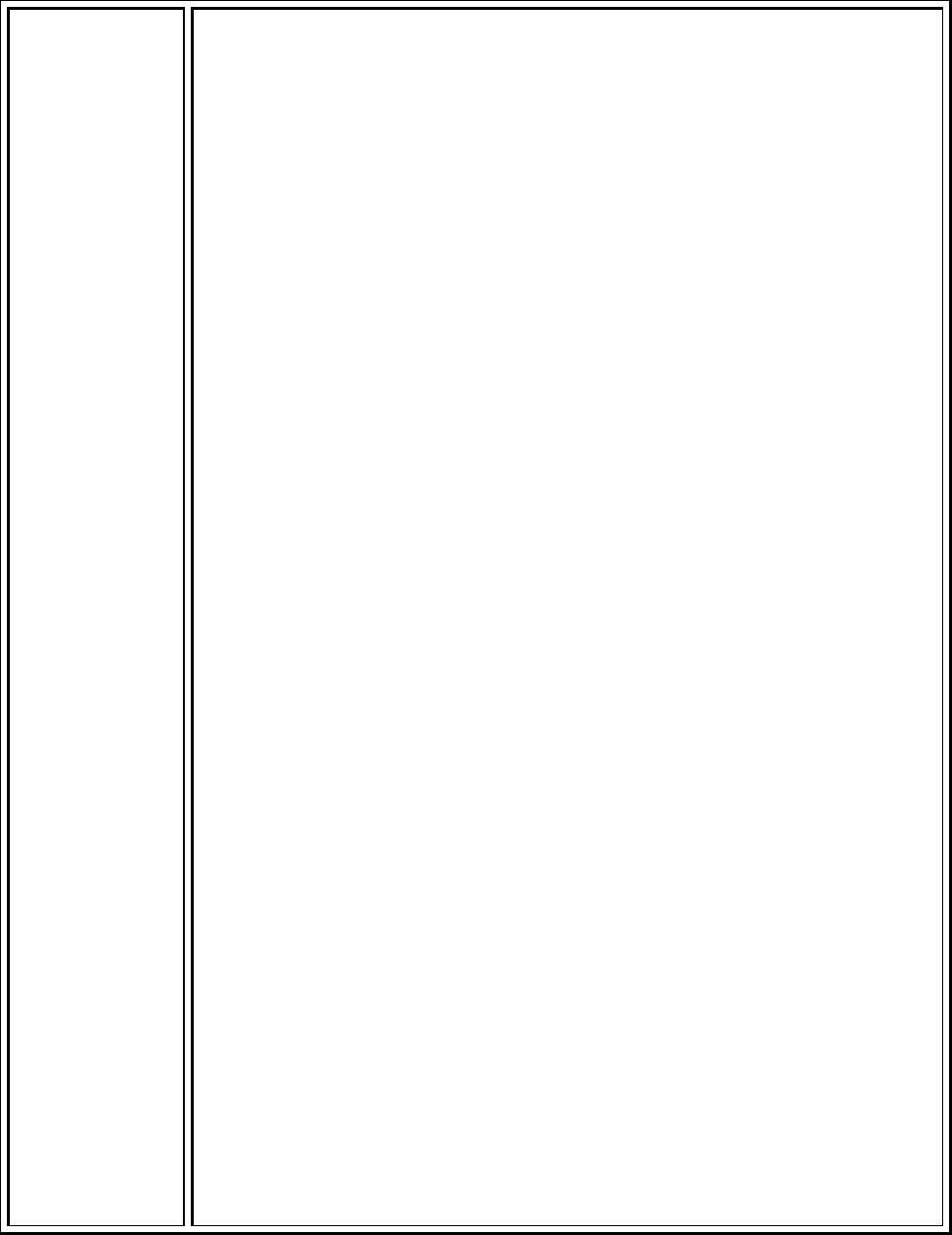
Transformational Leadership
Advocacy and Influence (7)
86
Information about these nurses remains posted on the Vanderbilt Nursing
Website. The 2010 award winners are listed below.
Spirit of Nursing Award:
Elliott Douglass, RN, BSN, WOCN
Monroe Carell Jr. Children's Hospital at Vanderbilt
What is the essence or heart of nursing at Vanderbilt? Several moving and
inspirational pieces were submitted, but the nursing council selected a
poem, submitted by Elliott Douglass, R.N., the wound ostomy and
continence nurse at Monroe Carell Jr. Children's Hospital at Vanderbilt.
Douglass, who spent most of her 13 years in nursing working with adult
patients at Vanderbilt University Hospital, says coming to work at Children’s
Hospital three years ago brought her love of nursing full-circle. It is a life-
long passion that began at the age of 3, when she developed epiglottitis and
nearly suffocated. She says James O’Neill, M.D., then chairman of Surgery in
Pediatrics, saved her life, and her experience in the critical care unit at
Children’s left a deep impression on her. Poetry has been another passion
for Douglass. “In high school, the boys would ask me to write poems they
could use to give to their girlfriends,” Elliott says with a laugh. Her love of
poetry and nursing blend nicely in the winning essay for the Children’s
Hospital “Spirit of Nursing” contest.
The Rebecca Clark Culpepper Award:
Jan Malone, RN, BSN
Interim Nurse Educator/Charge Nurse, Monroe Carell Jr. Children's
Hospital at Vanderbilt
The Rebecca Clark Culpepper award is given jointly by Vanderbilt School of
Nursing and Vanderbilt Medical Center Nursing to honor Becky’s many
contributions to both areas. The recipient can be a nurse at VUMC or faculty
at VUSN. The recipient of this award exhibits mentorship of fellow nursing
staff, faculty or students and actively promotes of the nursing profession.
There is a commitment to professional development at all levels.
In December 2009, Jan accepted the Interim Nurse Educator position for the
Pediatric Surgery and Adolescent Unit. Jan had agreed to support the unit in

Transformational Leadership
Advocacy and Influence (7)
87
this role as temporary position while the regular Educator is out on
maternity leave. During her short time in this role, she has been active in
attending clinical practice and policy meetings. She actively seeks out
evidence based research, collaborates with the management team, and
seeks staff input to support her recommendations. In addition to this new
role, Jan is an active member in the Society of Pediatric Nursing and has
recruited many new members into the organization. Recently, Jan was
confirmed as the new Vice President for the Middle Tennessee Chapter of
Pediatric Nursing. She attended the National Society Pediatric Nursing
Conference in Orlando, Florida this May.
In her Interim Nurse Educator role, Jan assigns preceptors to orient new
staff, pediatric nurse residents, and nursing practicum students and also
coaches and mentors the preceptors and helps them individualize plans to
meet the needs of the new staff members and students.
Jan encompasses the true spirit of nursing through her passionate
commitment to elevate the nursing profession and her commitment to her
colleagues. This is demonstrated through her quest to engage others to join
nursing organizations and seek continuing education opportunities that
advance nursing practice and organizational standards.
Vanderbilt School of Nursing Faculty Award:
Clare Thomson-Smith, JD, MSN, RN, FAANP
Assistant Professor of Nursing
Director, Center for Advanced Practice Nursing and Allied Health
This award is given to the Vanderbilt School of Nursing faculty (nurse or non-
nurse) who has made the greatest contribution to the field of nursing.
Clare Thomson-Smith serves as a role model, advocate and a mentor at the
School of Nursing, the Medical Center and the Tennessee Nurses
Association. She contributes to the academic mission of the school by
facilitating courses for the much-in-demand Health Systems Management
program of study – teaching students from around the country who are or
will become nurse administrators and leaders for health systems throughout
the country. As director of CAPNAH which is dedicated to supporting existing
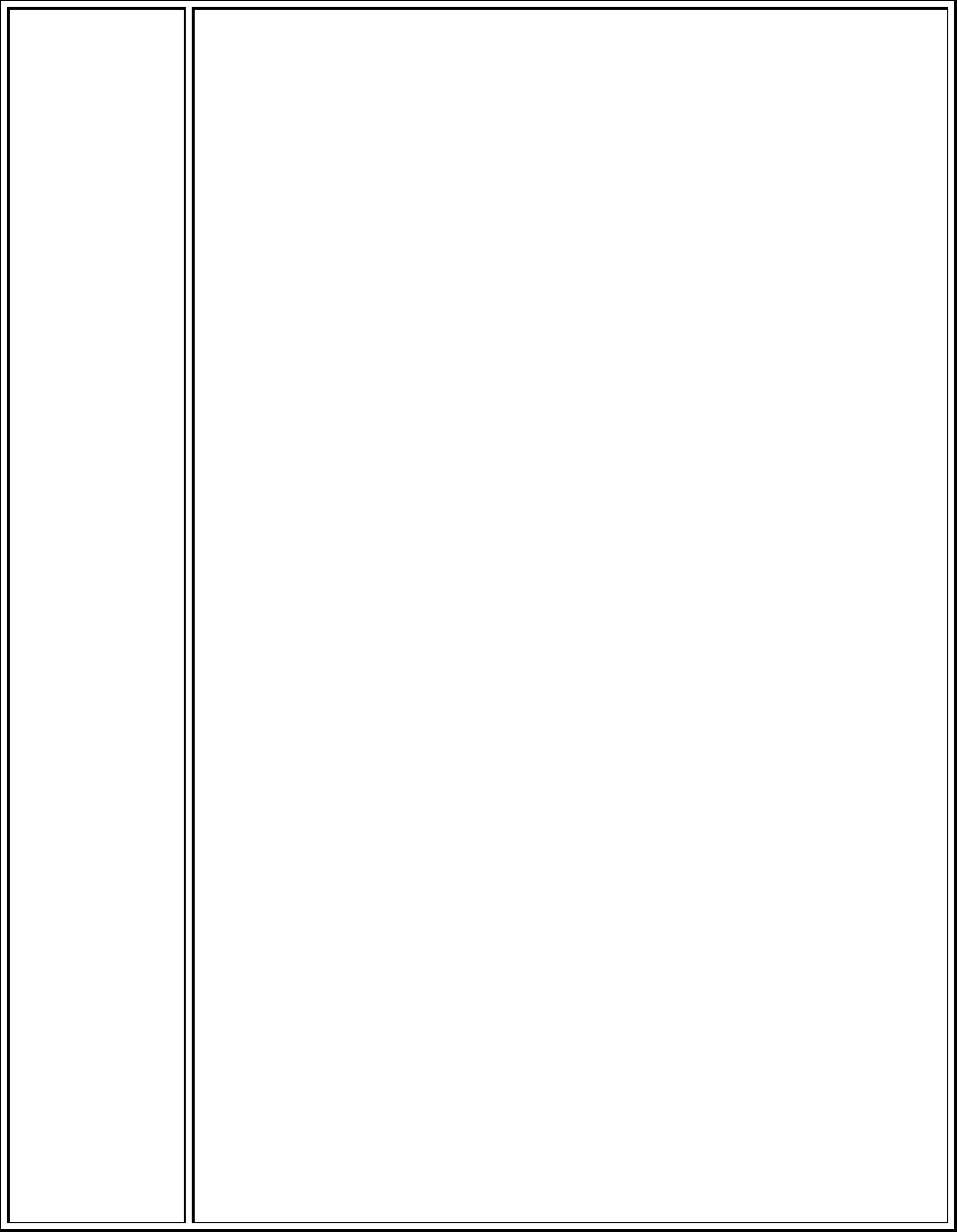
Transformational Leadership
Advocacy and Influence (7)
88
and emerging practices, she and her team have made significant strides in
mentoring advanced practice nurses and allied health professionals into the
profession and the VUMC culture with a robust array of activities and
professional development opportunities.
She has used her J.D. degree to become an advocate for policy development
related to advanced practice nursing. She serves as chair of government
affairs and health policy committee for the Tennessee Nurses Association
and can navigate the often challenging and ever-changing landscape of
health care legislation in the state. She voluntarily contributes her time to
these efforts to support the role of advanced practice nursing because she
believes in the important role that advanced practice nursing plays in health
care delivery – throughout Vanderbilt, the state and the country. Thomson-
Smith is widely viewed as an expert in her field and was recently selected as
a 2010 Fellow of the American Academy of Nurse Practitioners, recognized
for her outstanding contributions to health care through clinical practice,
research, education or policy.
Advanced Practice Nurse of the Year Award:
Kimberly Huffman, RN, MSN, PNP
Pediatric Otolaryngology
Kimberly is the Vanderbilt Children’s Hospital resource for the Pediatric
Otolaryngology service. She provides continuity of patient care by
participating in daily team rounds and attending rounds, evaluating
consultations in the ER and with inpatients, and facilitating preoperative and
postoperative care of patients. Although Kimberly joined the Peds ENT team
in 2008, her knowledge and clinical skills are well beyond expected for her
years of training. Kimberly confidently assists in patient management and
instructs residents how to care for common pediatric otolaryngology
problems. She is a huge resource for ensuring proper multidisciplinary care
of pediatric patients. She maintains open lines of communication with the
Pediatricians, Peds GI, Peds Pulmonary, PICU, NICU and ER. In addition to
these duties, Kimberly serves at the tracheotomy resource for Children’s.
She provides education to nurses, patients and families and ensures that the
necessary equipment and supplies are available prior to discharge. In fact,
she is often contacted to serve as a tracheotomy resource for patients not
Transformational Leadership
Advocacy and Influence (7)
89
treated by the Otolaryngology service. In addition, she has developed the
website for the Peds ENT department and her efforts there are decidedly
centered on patient understanding and care.
Kimberly has created and implemented several new evidence-based practice
(EBP) order sets for the Peds ENT service (including postop cleft lip, postop
cleft palate). She was also instrumental in developing a Children’s hospital-
wide, standardized post-tracheotomy order set. Kimberly also serves on the
Nursing Research Committee.
Kimberly is an integral part of the Pediatric Otolaryngology team. She is a
patient advocate, and provides seamless continuity of care from the clinic
and OR to the hospital. She educates residents and nurses on a daily basis
and is a Children’s-hospital wide resource for tracheotomy patients. Through
her collaborative efforts with other services, Peds ENT patients receive the
best care possible.
Staff/Unit/Department Educator of the Year Award:
Kara Gordon, RN, MSN, Nurse Educator
Vanderbilt University Hospital Medical Intensive Care Unit
The recipient of this award demonstrates participation in and models lifelong
learning and positively reflects the image of nursing. Education is Kara’s
passion. She is a positive, knowledgeable, cheerful and caring person. Kara’s
main focus is providing the staff with the tools needed to deliver excellent
patient care. She fulfills this challenging task while remaining positive and
helpful.
All aspects of Kara’s work are based on evidence. She models and promotes
evidence-based nursing practice, while coaching the staff in obtaining and
using evidence. She also collaborates with the EBL librarians in obtaining
needed information and utilizes critical care research from the National
Teaching Institute. Through the utilization and sharing of evidence, Kara is
able to influence nursing practice on the unit and organizationally.
Kara plays a leadership role in both unit and organizational initiatives,
including, but not limited to, blood stream infections, Pressure Ulcer
Transformational Leadership
Advocacy and Influence (7)
90
Prevention, nurse resident education, HINI, bariatric equipment and the
work around the Critical Care Tower. Helping to maintain a calm
environment when anxiety was very high supported the staff to focus on
safe patient care. Kara has been a leader in the work around the Critical Care
Tower. She was instrumental in developing the education provided to all
critical care nurses prior to the move and opening.
Kara is an advocate and support for the staff in regard to professional and
personal educational goals. She mentors staff in studying for and taking the
Critical Care RN certification exams and helps them obtain study materials.
Kara encourages staff to become certified in CVVHD for our renal
population. She works with graduate students and also took a refresher
pathophysiology course recently at Vanderbilt. Kara encourages staff to
continue their education whether it is graduate work or other.
Kara is a valued role model and colleague to the staff of the MICU and many
others throughout the Medical Center and also a great friend.
Julie Foss, RN, MSN, NE-BC
Nurse Manager, Medical Intensive Care Unit
Julie has been the manager in the MICU for 21 years and some of the staff
has been with her the entire time! Her hard work, dedication and nurturing
spirit have helped to create the awesome work environment in the MICU
today. MICU staff believes she is one of the finest leaders. Julie is a role
model for shared governance. She sets a tone of enthusiasm and inclusion.
Each staff member knows their comments and ideas are valued. Through
unit board, staff meetings, frequent emails, Friday communication, rounding
and general visibility, staff are able to provide feedback and stay informed
about the Medical Center and MICU.
Julie recognizes other departments’ contributions to patient care and urges
the staff to show appreciation to those who support patient care. Recently
she shared how a member of our Environmental Services team went above
and beyond the call of duty to help with a challenging patient. As a result,
we were able to celebrate and honor the ES staff member. She co-chairs the
Retention and First Two Years Retention Committee for Be the Best. She is
Transformational Leadership
Advocacy and Influence (7)
91
also active in HED Advisory, UTI Advisory, Falls Prevention, Handiworks, VAP
Dashboard, and Rapid Response. Julie helped lead efforts in transitioning to
the new Critical Care Tower.
Julie treats all people with respect and compassion. She lives the Credo and
is positive and inspires the staff to do the same.
Licensed Practical Nurse of the Year Award:
Arthur Thompson, LPN
Neurology Clinic
Our staff fondly refers to Arthur as "Mr. Vanderbilt.” Over Arthur’s thirty-
five years at the Vanderbilt University Medical Center, he has been in the
forefront of many great activities that have helped to make this institution
the place is it today, through Nursing. Some things Arthur has been a part of
are: the first Unit/Clinic Board in our clinic (and is presently the Unit Board
Chairperson); a leader in feeding the staff and the patients’ family members
on Thanksgiving Day in the Neurology units; advocating for the LPN name
badge change; a member of the original Nursing Staff Council, and
instrumental in the need to expand and develop a clinic nurse council to
better represent the outpatient nurses.
Although for many years, Arthur has been a mainstay in the Stroke division
of the Neurology Clinic, he is also a part of the Movement and Headache
team in the Neurology Clinic. Arthur continues to be an alternate for VMG’s
Nursing Staff Council as well as alternate for the Nursing Staff Bylaws
Convention Delegate.
This year Arthur Thompson has been appointed to the Tennessee State
Board of Nursing, and he is one of only three licensed practical nurses on
this important board. This appointment honors the role of the LPN and
instills pride for all Vanderbilt Nurses. Arthur is the type of nurse that makes
Vanderbilt Nurses stand out and his work contributes to making us a Magnet
designated organization. Arthur is a good friend to both patients and staff.
Research and Evidence Based Practice Award:
Donna Christensen, RN, BS
Evidence Based Medicine Specialist,
Transformational Leadership
Advocacy and Influence (7)
92
Case Management Department
In Donna’s role as an EBM Specialist, she meets the criteria for this award
many times over on a daily basis. Since 2008 Donna has served as a leader
on the Nursing Research Committee to build resources that support staff to
access nursing literature, conduct critical analysis and make practice
recommendations.
Donna supports many nurses in their quest through individual consultation
and the development of web-based EBP tools. One example is the “Got a
Question” tab on the Nursing Research web site. Nurses or any member of
the team can post a clinical question and receive a summary of the evidence
available to answer the question. The traffic in this activity is very high and
Donna has a personal commitment to provide high quality answers. A large
number of nurses have benefited from Donna’s extra efforts and thus
supporting quality patient care. Donna does work with the research staff in
the Eskind Biomedical Library on the complex questions, but screens each
one herself. Donna is a role model on providing feedback and presenting
her opinion.
Donna compiled all of the Research website links and for the search tips
section. This has given any nurse at Vanderbilt access to many resources
which provide evidence to support or improve patient care. Donna’s
greatest contributions may not lay within the realm of research itself, but
her evaluation of the implementation process. This evaluation process is
critical for us to continue to improve nursing practice at Vanderbilt as well as
move the science of nursing forward. Donna has been a leader in the efforts
to move Vanderbilt nursing to a higher level of evidence-based practice. Her
contributions to the Nursing Research Committee are invaluable and
showcase only a portion of Donna’s dedicated work
Team Award:
Monroe Carell Jr. Children's Hospital at Vanderbilt
Perioperative Services Guatemala Mission Team September 2009
Each year throughout the Medical Center, different individuals and teams
travel the U.S. and the world on medical missions. Several teams have gone
to Guatemala and we salute all of those teams and individuals. The
Transformational Leadership
Advocacy and Influence (7)
93
particular team being recognized by this award is the Guatemala Team of
September 2009.
The success of this team’s hard work is measured in the quality of the lives
changed; specifically the children of Guatemala. From the 96 patients
screened to the 51 who received surgical care, this team had a direct impact
on the quality of life for many. Surgical outcomes were measured by clinical
data, but cannot compare to the emotional well-being. The clinical
outcomes are followed by both The Shalom Foundation and individual
physicians at Vanderbilt. They were also able to follow-up on past surgical
patients and bring that news back to other staff from previous mission trips.
The team demonstrated a strong sense of inquiry in preparation for the trip
by packing all necessary equipment and supplies and taking into account
cultural aspects as well. Coloring books and candy were mixed in with
surgical drapes and scalpels. Spanish translation of teaching materials was
instrumental to the team’s success. None of this could have been
accomplished without research and team coordination.
The interpersonal communication skills team members honed have
improved “hand overs” here at Vanderbilt. In addition, team members
reported they got back to the basics of nursing, through having to “make
do” and be creative. Working with the staff from the local hospital was
rewarding for the team and enhanced learning on both sides. Their
welcoming attitudes taught the Vanderbilt team a lesson in
inclusiveness. The team faced challenges and overcame many obstacles.
However, it was worth it to see the smiles and to receive the handshakes
and the hugs. Changing lives in a different country means changed lives back
here at Vanderbilt.
Rosamond Gabrielson Staff Nurse of the Year Award for Monroe Carell Jr.
Children's Hospital at Vanderbilt, Vanderbilt Medical Group, Vanderbilt
Psychiatric Hospital, and Vanderbilt University Hospital
Lisa Foust, RN, Vanderbilt Medical Group, Vanderbilt Health One Hundred
Oaks
Transformational Leadership
Advocacy and Influence (7)
94
Lisa Foust has defined the model for "team approach." Her colleagues
respect and admire her. They turn to her for patient care advice routinely.
Lisa treats every patient as her own, and leaves nothing for the next person
to finish. Lisa's friendly and confident demeanor immediately establishes a
good rapport with patients. But what she offers our patients is far more than
a great first impression. To them, she is a reliable and loyal advocate who
inspires trust and confidence. She is central to their success in blood
pressure management, weight loss, dietary and exercise compliance, and
lipid management, as she is integral to the follow-up on these patients both
in clinic and in the interim between clinic visits.
Lisa has been integral to the success of the Vanderbilt Heart Preventive
Cardiology program. In only two short years Lisa has become so
knowledgeable about management of cardiovascular risk factors that she is
able to anticipate the next step (e.g. changes in medications) and prepare
for it, and she frequently makes pertinent suggestions for patient care and is
able to integrate complicated factors like cost, likelihood of patient
compliance, side effects, and/or drug-drug interactions into her decision
making suggestions. Lisa has promoted preventive cardiovascular health,
women's health, and Vanderbilt, and she continues to self-educate. She
attends evening Vanderbilt Lipid Club journal club meetings regularly and
she served as a host at several OHO opening events to promote the new
clinic. She has also been critical in helping design and implement a free
(daily!) heart health screening program for women at OHO (this program
could serve 500-1000 women per year).
Lisa makes many contacts with other RNs and practitioners to constantly
stay involved in what is going on in preventative medicine. Lisa is also the
frontline contact for the preventative program's involvement with the lipid
management practice. She works with that team's NP, MDs and research
team to ensure that patients who qualify for new and ongoing research
studies are entered and have assistance.
Lisa Foust is the absolute epitome of nursing. She is an incredible and loyal
colleague. She is a patient advocate, and her leadership style is organized
and thorough. Her impeccable work ethic, leadership, thoughtful approach
to patient care, and contribution to Vanderbilt deserve not only recognition,

Transformational Leadership
Advocacy and Influence (7)
95
but great reward.
5 Pillar Leader
Award
Two nurse leaders this year were honored by the entire organization as 5
Pillar Leaders. All leaders serving VUMC are eligible with the exception of
executive leadership guided by the following criteria:
Nominees in a leadership position for at least one year.
Nominees must be in good standing and nominations must be
supported by “one up” leader.
Nominations may be made by any faculty or staff member. Self-
nominations are not accepted.
Nominees must demonstrate consistent practices that impact
success across the five pillars and demonstrate consistent Credo
behavior
The following excerpt was taken from the Reporter and written by Paul
Govern
9/25/2009 - Several staff and faculty who do consistently outstanding work
were honored last week at Vanderbilt University Medical Center's
Leadership Assembly at Langford Auditorium.
Donna Williams, MSN, R.N. NEA-BC, an administrative director with
Operative Services, was presented with the Five Pillar Leader Award for
superior
All-around leader Donna Williams, R.N., received a Five Pillar Leader Award.
(photo by Susan Urmy)
Performance across VUMC's management “pillars” — employee satisfaction
and retention, service, quality, finance and innovation — and for upholding
the VUMC Credo.
The award was presented by John Brock III, M.D., surgeon-in-chief at the
Monroe Carell Jr. Children's Hospital at Vanderbilt.
Transformational Leadership
Advocacy and Influence (7)
96
“Donna Williams is simply the best of the best. She makes everyone around
her better. There's no greater honor for someone like me than to work with
someone like Donna,” Brock said.
December, 2009 Karen Hughart, M.S.N., R.N., director of Systems Support
Services, was presented with the Five Pillar Leader Award, which recognizes
superior performance across the Medical Center's management “pillars” —
service, quality, finance, people and innovation.
Karen Hughart, M.S.N., R.N.
As director of Systems Support Services, Hughart has aided clinical
information technology implementation at VUMC. Over many years, she and
her staff have had a hand in Vanderbilt's growth as a clinical information
technology powerhouse.
“Karen's dedication to her staff is remarkable,” the award nomination
stated. “She never fails to demonstrate respect and consideration for others.
She is known to many seasoned Vanderbilt nurses as 'the best manager I
ever had.' … Karen embraces the sense of ownership that is key to the
Vanderbilt Credo.”
Reward and
recognize
System
Vanderbilt offers a method for leaders to reward and recognize staff
through the Reward and recognize System. The system is an electronic one-
stop shop for rewards and recognition! This year the system was open to
colleagues who can now more easily recognize each other with Life
Occasions E-cards or Performance E-cards to simply say “congratulations on
the new baby” or “thank you for your efforts”.
RECOGNIZE awards will be issued by award givers through
MyVUMCRecognition in the form of points. Points can be saved or spent in
Transformational Leadership
Advocacy and Influence (7)
97
our Universal Rewards Mall which offers over 5,000 merchandise items and
numerous gift cards.
Credo Award The Credo Award recognizes staff and faculty who exemplify the Medical
Center's standards for service and all-around professionalism, while the Five
Pillar Leader Award goes to those who exemplify Medical Center leadership
standards. Awards are bestowed each quarter.
The Credo Award went to Edie Vaughn, R.N., staff nurse (on 9 South)
Edie Vaughn, R.N.
“'Edie spoils everyone she comes into contact with. She's such a joy to work
with and to watch her welcome every patient with her smile.’ … ‘Edie brings
warmth, laughter and insight to our workplace. Edie has been walking the
Vanderbilt Credo every moment of every day long before the Credo was even
published.'”
Orientation
Buddy System
Alaina Knight, staff nurse on 7 North was awarded the opportunity to
present a poster on the buddy system she helped develop on her unit at the
American Heart Association Quality forum. Expenses for the trip were paid.
[TL7-Exhibit B-1-Buddy System Poster-ONSITE] Alaina noted that when
nurses came out of orientation, they still needed support. They did not
always have the chance to experience or become competent in rare but
necessary care 7 north nurse are called to deliver. Alaina devised the “Buddy
System” for nurses out of orientation. After the RN is out of the typically 6
weeks of orientation the new nurse is paired with an experienced nurse. The
experienced nurse and the new nurse have assignments close together
geographically. The experienced nurse gets report form the new nurse and
checks on the new nurse every two hours. The experienced nurse is
responsible for monitoring, supporting, coaching the new nurse and stands
ready to assist in any moment. This was received with great reviews by staff.
The idea has been formalized in other units.
Nursing stress
management in
The PEDS ED has seen a tremendous amount of growth in the past 5 years
now seeing approximately 60,000 children annually. With growth comes an
Transformational Leadership
Advocacy and Influence (7)
98
the Pediatric ED increase in the number of traumatic injuries, newly diagnosed cancers or
other diseases, and deaths. The management team has been committed to
come in for every death for the past 2 years. Upon arrival, the management
team will assist the family, staff, and lead debriefings for the team. This
support has led to an increased awareness in staff for the need to “take care
of themselves” emotionally and physically given the stress factors of the job.
There have been many informal and formal debriefing for the team.
Gregg Horn, a staff nurse (who is now a Charge Nurse) was very passionate
about proactively managing the level of staff stress. He developed a stress
survey to get a baseline for the level of stress that the staff was
experiencing. His work and the support of the management team led to
more formal debriefing and an increase in visibility of EAP in the PED on an
ongoing basis. EAP now makes monthly rounds in the department for day
and night shifts to assist with the stress levels of the staff. This is in addition
to the debriefings that occur after an event.
The post survey results were very positive. The work has been transforming
how nurse manage stress. [TL7-Exhibit C-1-VCH ED Stress Project]
Daily shift to
shift staffing
report earns
Leann Grimes
Recognition
It can be difficult to plan the right staffing for a unit. It is especially difficult
when varying patient acuity requires many different nurses to patient ratios
all in the same shift. This is true in the OB/GYN inpatient unit which provides
care for post partum, ante-partum and GYN ONC patients. The AWOHNN
guidelines are used for staffing and to determine the nurse to patient ratios.
Even more difficult than creating the budget is managing the unit day to day
to ensure the appropriate care is provided within the budgetary plans.
Leann Grimes, charge nurse developed a daily management tool used by the
charge nurses to make the assignments based on acuity of the patients. The
tools tell the charge nurse how many nurses are needed and how to
balance assignments. The tool has been in use since 2008 and is extremely
effective. The Advisory Board recognized Leann for her work through a
Future of Nursing Award. Leann was recognized in the Frontline Leader
graduation and on the Vanderbilt Nursing Web site. [TL7-Exhibit D-1-Staffing
Sheet]
Vanderbilt
Professional
This program is fully reviewed in EP20. VPNPP is the professional
advancement program for clinical nurses at Vanderbilt. It is the way nurses
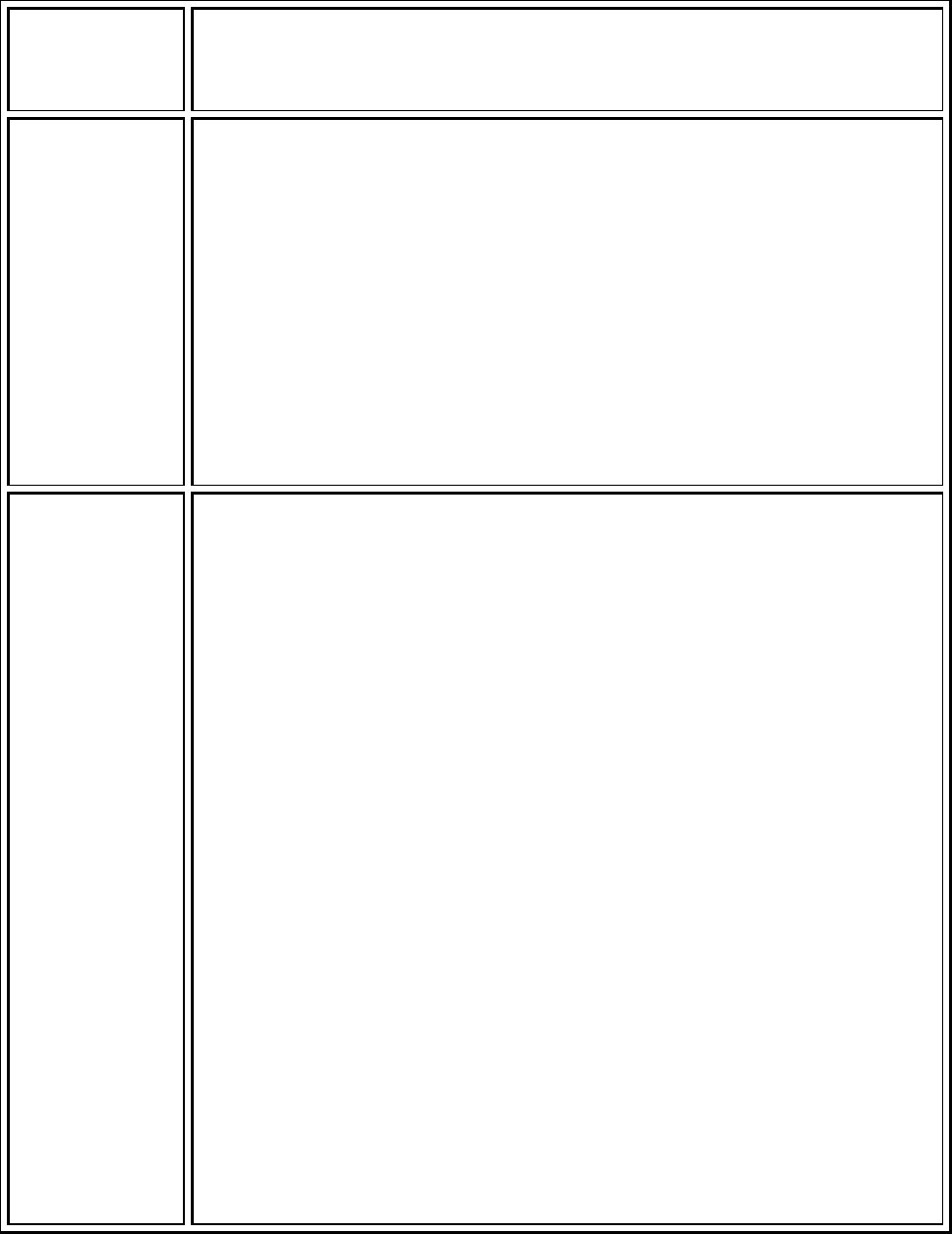
Transformational Leadership
Advocacy and Influence (7)
99
Practice
Program
are recognized for their excellence n nursing through promotion that allows
them to stay at the bedside. Both pay and title change as nurse’s advance in
this program.
Evaluation
recognition
All performance evaluations at Vanderbilt are performance based. Annually,
employees have an opportunity to be recognized for contributions above
the norm in the evaluation process. The evaluation rating scale is a 1-5
scale. A score of three is considered competent and meeting the expectation
of the job. A score of 4 is considered proficient and a score of 5 is considered
excellent and expert performance. Criteria established for level 4 and 5
include more leadership such as coaching and mentoring. It also includes
broadening influence in the organization through sharing of expertise. The
salary adjustments are consistent with the level of performance varying for
each staff member based on their evaluation score. See OO 17 for more
detail.
E
3
= Exploring
Executive
Excellence:
Building the
Legacy and
recognizing
future leaders
Among managers, there are some who will be the future of nursing. They
are among the best. In an attempt to recognized their talent and invest in
succession planning, a program has been developed to do just that. The
program for nurses stems from a focus on recruitment, retention, and
ongoing development of nursing leaders of as part of our Be the Best (BTB).
In November, 2008, the Director of Nursing Education and Professional
Development brought together a small subset of our BTB committees to
discuss what type of mentoring or coaching program VUMC should develop
for current or potential nursing leaders. Nurse managers had been
encouraged to pursue additional education and achieve certification but had
not been provided with formal mentoring. In addition, the majority of
nurses were pursuing advanced education in a clinical track with few
pursuing a leadership track.
Planning began in November 2009. The following committees and
departments had representation on this committee:
- Recruitment and Second Year Retention
- Leader Development
- Diversity
- Nursing Education and Professional Development
In addition, a few managers to participate on this planning committee to
provide their ideas and feedback about what a mentoring program include.

Transformational Leadership
Advocacy and Influence (7)
100
The committee determined the focus of a leader mentoring program should
be the development of nurse managers in preparation for administrative
roles. The objectives were to:
1. Ignite a passion for nursing leadership.
2. Attract talent to the Nursing leadership role.
3. Create an environment where emerging Nursing leaders recognize
that leading nurses is satisfying work and where nurses feel invited to
explore career opportunities.
4. Help nurses learn and apply the art and science of nursing leadership.
5. Transform a nurse’s passion for clinical excellence with individual
patients to a passion for creating environments for all nurses to
practice clinical excellence.
The work was informed by similar work at St. Barnabas Health System and
their willingness to share their program details.
The program launched September 7, 2010 and will annually offer 6
managers time, exposure and experience with members of the Nursing
Executive Board..
The pilot program will run for one year (September 2010 – September
2011). During the year long program participants will be required to meet
with each mentor for at least one hour. The participants are provided with a
portfolio of the Executives strengths as well as their own strengths
determined through the use of “Strengths Finders”. During that session the
participant should ask questions and will spend some time after each
meeting reflecting on several questions. (Provided TL7 – Peterman). The
participants are able to negotiate a more formal and long term mentoring
relationship with an Executive if they wish.
A formal evaluation has been designed for the pilot program.
[TL7-Exhibit E-1-E3 Overview, TL7-Exhibit E-2-E3 Mentoring Schedule, TL7-
Exhibit E-3-E3 Questions Example]
Interdisciplinary rounding and plan of care development in the CVICU recognized through
national presentations
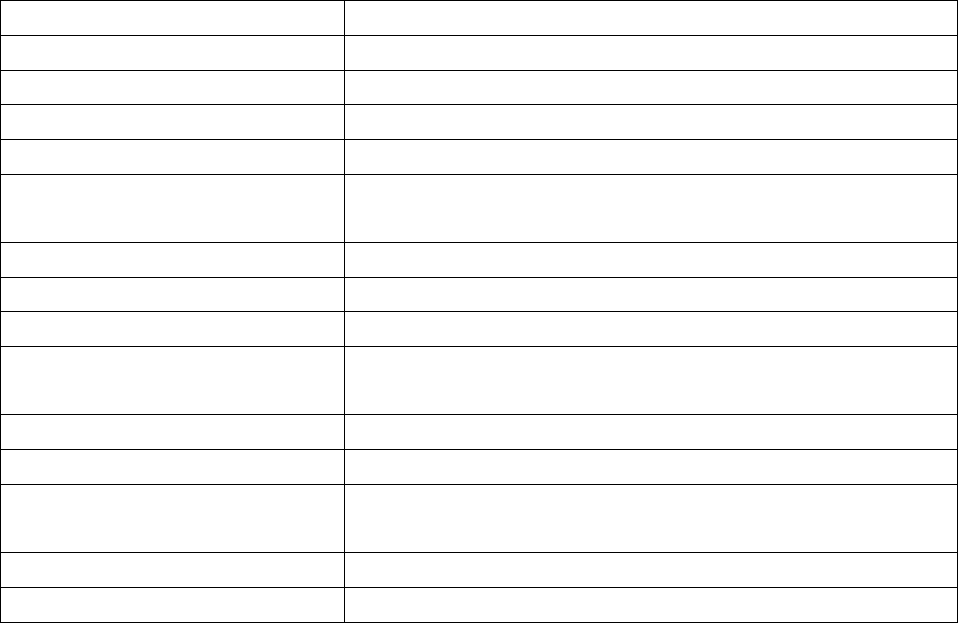
Transformational Leadership
Advocacy and Influence (7)
101
The following is an account of innovation that was recognized through presentations at national
meetings.
Table TL 7 – 2: Participants
Kathy Burns, MSN, RN CVICU Clinical Nurse Specialist
Jeannie Byrd, MSN, RN, NE-BC CVICU Manager
Kirk Krokosky, RN, CCRN CVICU Resource Nurse
Tonya Beattie, BSN, RN2, CCRN CVICU Staff Nurse
Jillian Russell, BSN, RN CVICU Staff Nurse
Brian Widmar, MSN, RN, APN,
CCRN
Cardiac Surgery Nurse Practitioner
April Kapu, MSN, RN, APN Cardiac Surgery Nurse Practitioner
Dr. John McPherson CVICU Medical Director
Dr. Chad Wagner CVICU Medical Director
Dr. Lee Parmley Director, Division of Critical Care/Department of
Anesthesiology
Anna Ambrose, RRT, MHA Administrative Director: Respiratory Therapy
Dan Johnson, Dph CVICU Clinical Pharmacist
Robin Steaban, MSN, RN Administration of Operations and Nursing/Vanderbilt Heart
and Vascular Institute
CVICU Unit Board
CVICU Staff
CAUSE/REASON FOR CHANGE:
An individualized plan of care was present in the patient record, but it was
compartmentalized into specialty notes, diagnosis-specific clinical pathways, and current order
sets.
This process frequently resulted in:
Missed or delayed communications and verbal relay errors
Care intervention and progression delays
Suboptimal utilization of the specialty expertise offered by team members
Transformational Leadership
Advocacy and Influence (7)
102
Lack of understanding of the reasons for ordered interventions – resulting in reduced
ability to apply prioritization and critical thinking skills while implementing and
evaluating care outcomes
Conflicting orders
Lack of patient and family understanding of the plan of care
Patient and family concerns that, with so many people involved, care coordination was
not occurring
HOW WAS IT DONE
This process has been ongoing over the last two years with constant review and
enhancements.
Phase I:
A “blank” interdisciplinary plan of care form was created with columns for initiation
dates, patient goals, evaluation codes (examples: met, continued, revised, discontinued) and
signatures. His approach and form originated in a hospital-wide, interdisciplinary committee
whose objective was to improve the creation (and evidence) of an individualized,
multidisciplinary plan of care. The CVICU agreed to be one of the pilot units. The form’s purpose
was to supplement, not duplicate, the goals presence on the diagnosis-specific clinical
pathways and to identify and track one to three of the patient’s priority, individualized goals.
In the CVICU, the form was primarily used to document individualized blood pressure, cardiac
output, incentive spirometry, activity, or nutrition goals set for the patient.
All members of the interdisciplinary team were asked to contribute to the form. It
quickly became a nursing-only form as other disciplines began rebelling against having to
“double document” their goals. Despite its failure as a document that was completed by the
interdisciplinary team, the CVICU nursing leadership team recognized that use of this tool
succeeded in demonstrating that individualized goals were being established by the team and
that goal prioritization was occurring.
The primary failures were:
Transformational Leadership
Advocacy and Influence (7)
103
Completing the form was not part of workflow. It was a separate work task. The form
was completed after the rounding and care planning process occurred because
completion was a performance expectation – not because the tool was a valued,
working document. The “real” care information was still in scribbles on the white
board, in the parameters written sideways in the margins of the nurse’s worksheet
during rounds, or in information jotted on a strip of “stuck down” silk tape during OR –
ICU handover reports.
The tool did not include a comprehensive plan of care.
The form directed that information be documented in “measureable goal” verbiage.
Nurses who are caring for patients with complex, multi-system, changing needs do not
actually think in complete goal statements. So, “the plans” are usually target parameters
and interventions. For example: Providing adequate nutrition is a goal for all patients.
Increasing tube feeding to a target of 75mL/hour without evidence of gastric distension,
diarrhea, or aspiration makes the generic nutrition goal measureable and individualized.
The working “goal” for the busy nurse is actually the intervention to “increase tube
feeding rate to 75 mL/hour as tolerated”. The rest is known. Repetitive documentation
of this information for all patients is considered to be academic and without true value.
It detracts and reduces compliance.
PHASE II:
The underlying objective of the quality initiative was to improve interdisciplinary care
planning, to ensure that plans of care were comprehensive and clearly communicated, and to
ensure that progress toward meeting goals was timely and ongoing.
Therefore, Phase II of this project expanded to include:
1) Restructuring of the Rounding/Plan of Care development process in the CVICU. This
included redesign and standardization of the rounding format to achieve effectiveness and
efficiency. All members of the team should have opportunity to contribute, but this
needed to be accomplished without concurrently extending rounding time. Designing this
process was challenging because the CVICU is a mixed CCU/Cardiac and Vascular Surgery
unit with two rounding teams: One lead by rotating Intensivists with consistent NP/PA
providers and one lead by rotating Cardiologists with rotating Residents. [TL7-Exhibit F-1-
CVICU Rounds Pocket Card]
2) Redesign of the Plan of Care form to include: [TL7-Exhibit F-2-Plan of Care (Instructions)]
Transformational Leadership
Advocacy and Influence (7)
104
a) Designated, labeled spaces for multi-system/multi-focus goals and interventions
b) Checkboxes for select quality focuses to reduce oversights (Examples: DVT prophylaxis
ordered, bowel regime ordered, and daily review of need for lines/tubes done)
c) Dedicated space to indicate the patient’s status on the clinical pathway so that there
would not be a need for multiple record entries to complete goal achievement
documentation. The clinical pathway still provides the foundation for the plan of care.
The form is used for individualization of the plan when a diagnosis specific pathway is
present; it provides the complete plan of care when a pathway is not available.
d) Removal of the requirement to document the plan in formal, measureable goal form.
3) A process design that ensured that the bedside nurses would be active participants in
multidisciplinary care planning and not just data reporters and recorders. Bedside nurses
assess and evaluate progress or regression from pathway and goal achievement on an
ongoing basis. It is nonsensical, nonproductive, and professionally-demoralizing to exclude
nurses from this process during physician-led rounds. [TL7-Exhibit-F-3-CVICU RN Handover
Report]
4) Redesign and standardization of the unit’s RN-RN handover form to provide more structure
and consistency for information transfer. This became integrated into the overall project
because a better system for information transition was needed to help the newer nurses
feel better prepared (and thus more confident) for their role in rounds and to help to focus
the “ramblers”. AM rounds start immediately after change of shift. Any nurse can feel
unready to provide comprehensive information about a new patient and his/her needs
when they have just assumed care and have not yet completed a full assessment.
5) An initial RN-RN handover tool was drafted by the CVICU CNS by combining features from
forms originally created by staff nurses for personal use and from forms created by RN
preceptors to help their new orientees get organized, ask the right questions, and provide
the right information during handover reports. The handover form was/is two pages. Page
one is an ongoing record of the patient’s invasive lines and significant procedures. It is
designed to provide quick access to key information (without repeatedly searching the
record) and to assist with comprehensive reporting on complex patients. Page two is
designed for transition of current assessment and order information. A new page two is
used for each handover. Form use was endorsed by the CVICU Unit Board and peer
Transformational Leadership
Advocacy and Influence (7)
105
education and coaching was provided. After several months of use, a page two revision was
spearheaded by a staff nurse. Input from all CVICU nurses was solicited by the staff leader.
More preprinted, circle, or fill in the blank options were added. Checklists for select, staff-
identified, high risk handover details were incorporated. The revised form was approved for
implementation by Unit Board.
Key elements of the expanded process included better preparation by nurses to
participate in rounds (new RN-RN handover forms), incorporation of plan of care
documentation into the workflow process, a more comprehensive, multidisciplinary plan of
care (new plan of care form and new, standardized, expanded rounding team and format), and
a summation. At the end of rounds, the nurse reads back the plan of care. This ensures that
nothing has been missed or misinterpreted. Because we are a University hospital, rounds are
teaching opportunities. This results in suggestions and discussions that may be generalized.
The read-back helps to ensure that the nurse, the person who is responsible for implementing
and coordinating the plan, is clear.
OUTCOME:
This very important, but complex improvement initiative was started two years ago.
Parts are hardwired and require little ongoing support, but it is still (and may always be) in
evolution and improvement mode. The rounding and plan of care development processes are
firmly implanted with the cardiac and vascular surgery patients, but the rounding format is not
as consistent with the cardiology patients. The Residents on the Cardiology service rotate
monthly and process success relies heavily on the Cardiologist leader, how long the Residents
have been on service, and the confidence/assertiveness of the staff nurse participant. Pre-
service meetings have begun with the Cardiology Residents. Expectations for the rounding
process and plan of care development are now part of their unit orientation. Laminated pocket
cards describing the process and delineating role responsibilities for rounding and plan of care
development are available.
Part of the initiative is to consistently involve the patient and family in rounds and plan
of care development. Patient and family inclusion is increasing, but is still variable and quite
dependent on the Attending Physician or Intensivist who is leading the rounds.
Nurses are now consistent participants in AM rounds. If they do not join the rounding
team, the team seeks them out. A comprehensive plan of care is consistently documented
during morning rounds. During the abbreviated evening rounds, the plan of care is evaluated
Transformational Leadership
Advocacy and Influence (7)
106
and, if needed, modified. Although goal achievement and plan modification are now
consistently discussed, documentation of the evening revisions on the plan of care form
remains an improvement opportunity.
The new plan of care is initiated immediately after rounds. Previously, key aspects of the
plan were unknown until orders were entered and reviewed. Discussion of the plan of care
(including consult input) includes resolution of conflicting orders. The process is also assisting
with intervention sequencing and prioritization.
An unexpected outcome of this process has been the identification of some behavioral,
delay patterns with specific nurses. Example: When the plan includes removal of lines or
catheters and the plan is read back to the team, repetitive intervention delays become evident.
These delays are being recognized and reported.
EVALUATION
Direct observation of the rounding process
Audit of the Plan of Care Forms
Feedback (solicited and unsolicited) from the Nurses, Physicians, Residents, Nurse
Practitioners, and other team members
INFORMATION SHARING
Processes and forms were shared with other Vanderbilt ICUs at the Institutional Critical
Care Committee
Poster presentation at the 2010 ACCA Cardiovascular Administrators' Leadership
Conference in Atlanta, Georgia
Presentation at the UHC Cardiovascular Council meeting in the Fall of 2009 at Duke
University
[TL7-Exhibit-F-4-Poster-ONSITE]
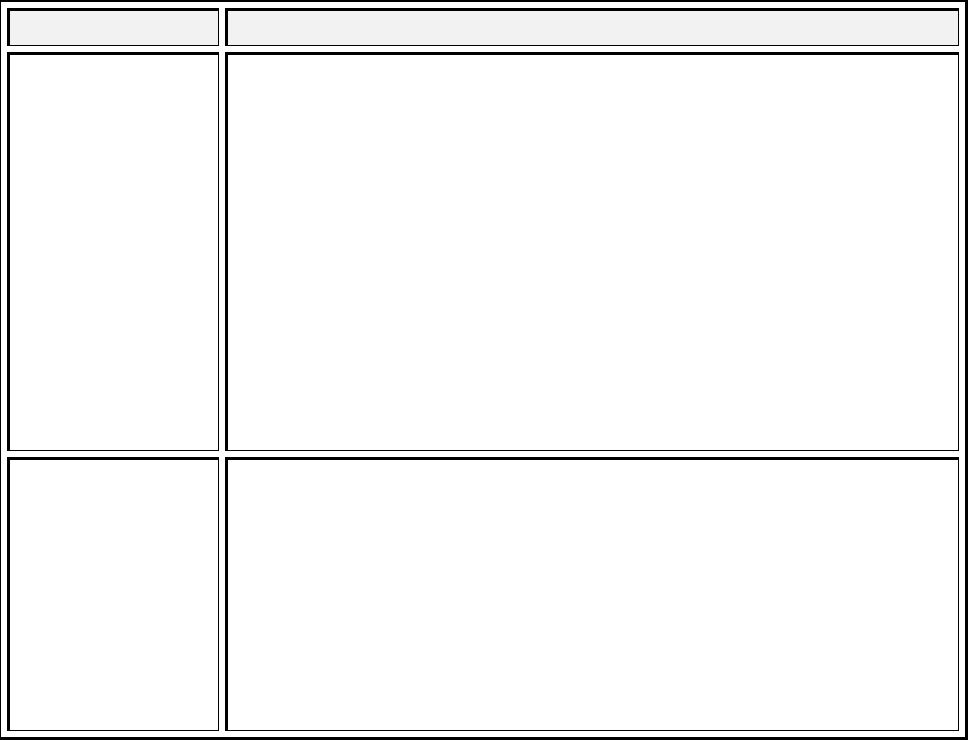
Transformational Leadership
Visibility, Accessibility and Communication (10)
107
Visibility, Accessibility, and Communication
Source of Evidence 10
Describe and demonstrate how nurse leaders use input from direct care nurses to improve
the work environment and patient care.
There are multiple ways nursing leaders have access to staff nurses and respond to
information from them to improve the environment nurses work in and the resulting patient
care. Through staff meetings, unit boards, leader rounding, staff nurse councils leaders learn
what barriers exist to patient care and ideas staff have t improve equipment, systems and
processes. The following demonstrates the request and the leader and organizational response.
Table TL 10 – 1: Request/Response
Input from Nurse(s) Leader Response
Vital Signs changes
Jon Coomer, the manager of the psychiatrics VITA/Adult 3 unit gathered
information from staff related to work flow issue. Some of the feedback
given was that all patients were required to have vital signs at 6 a.m.
regardless of their clinical condition. This was a concern to patients and
staff and added little clinical advantage. The MD’s did not round until 9
a.m. so the vital signs were not relevant from 6 a.m. for clinical decision
making and often had to be repeated. A group of staff redesigned shift
responsibilities to allow the day shift to absorb this work. [TL10-Exhibit-A-
1-VITA Daily Schedule] Both staff and patients verbalized appreciation for
the change and it has had no noted affect on management of patient’s
clinical issues.
Myelosupression
preceptor
improvement
A nurse on the myelosuppression noted the need for improvement in the
orientation program. The Manager supported her efforts to improve the
orientation through guidance, coaching and mentoring. The manager
used the opportunity to help the nurse develop new skills and to meet
the needs of the unit. The nurse convened a preceptor group to review
the orientation of new hires. The group surveyed staff about their
perceptions of orientation and then informally surveyed the preceptors.
From these experiences, there were several suggestions for
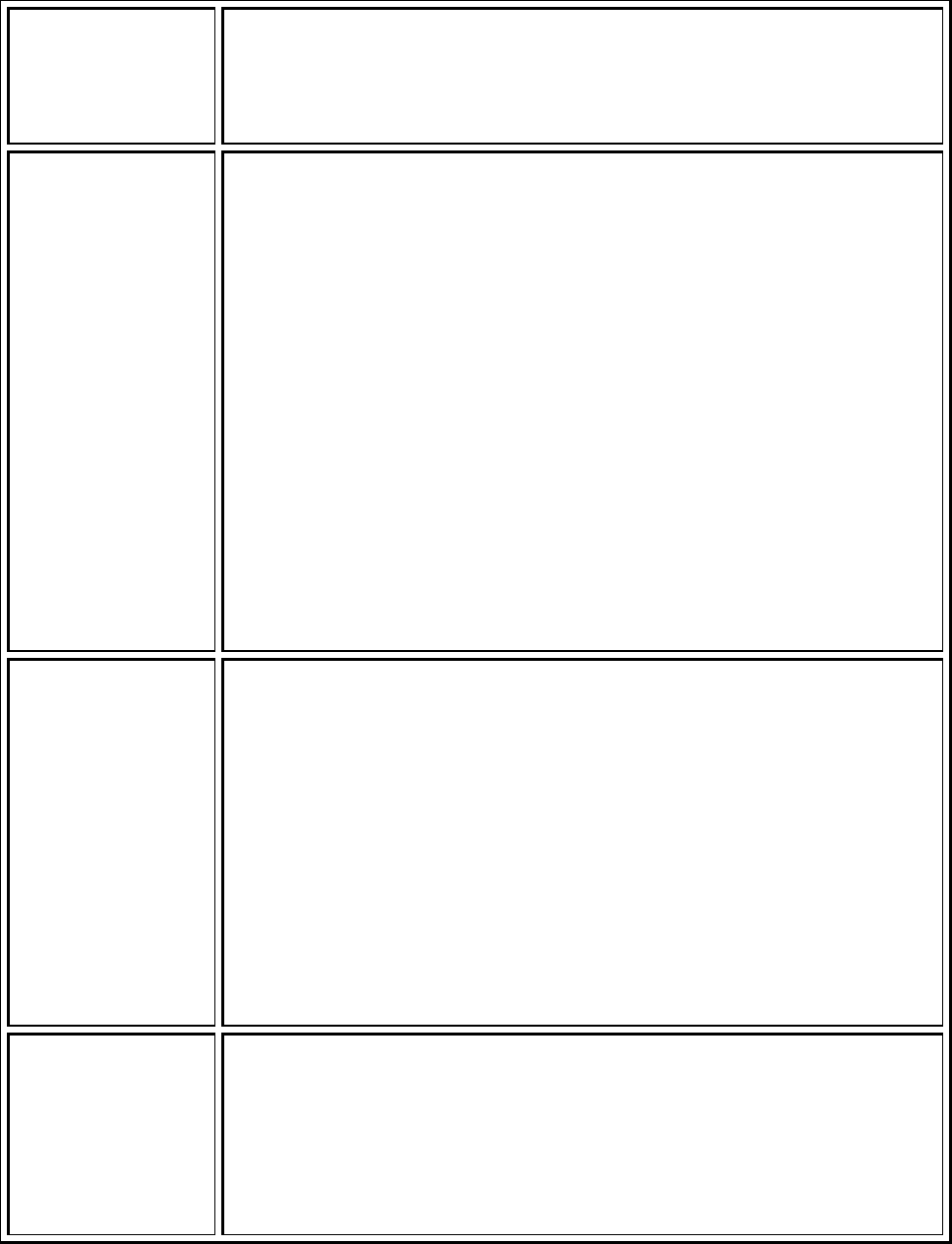
Transformational Leadership
Visibility, Accessibility and Communication (10)
108
improvement in orientation. Those included: Development of an
orientation checklist, teaching sheets of common medications and
procedures, list of frequently used phone numbers; 10 rules for all 11
North staff. [TL10-Exhibit-B-1-Meeting Minutes]
Targeting clinical
growth in the
Neonatal intensive
care unit
The NICU staf
f
s were concerned that they were not getting assigned to
the right patients for them to get exposure and gain experience in clinical
areas where they needed development. A spreadsheet exsisted that
identified which nurses were competent in which skills and this was to be
used as a guide for the charge nurses in making assignments. In a
complex 76 bed unit, charge nurses found the use of the tool difficult and
nurses were still not assigned to patients that would allow them to learn
new skills. In a charge nurse meeting they identified that a white board
could be placed in the charge nurse office with the necessary skills listed
at the top. Staff would be encouraged to write their names in the column
where they needed experience. [TL10-Exhibit C-1-Charge Board Photos,
TL10-Exhibit C-2-Mentorship Charge Meeting] Charge nurses could “at a
glance” know who needed what experience and make assignments
accordingly. Staff nurses have expressed greater satisfaction in getting
assignments that help build their skill since this change took place.
Bone Marrow
transplants and
discharge needs
A staff nurse on the Myelosuppression unit was concerned that patients
were not being prepared adequately and consistently for discharge. The
staff nurse discussed her concerns with the casemanager and the
management team. The manager supported the staff member through
coaching and mentoring to meet the developmental needs of the staff as
she developed a discharge checklist. After a trial use of the checklist on
her own patients, she found she was able to identify discharge issues
earlier allowing early intervention. The manager used this small test of
change by one nurse to improve the discharge process for all patients.
In-services are in progress (October, 2010) for all staff to begin to use the
form. [TL10-Exhibit-D-1-Discharge Checklist]
Staffing Changes 11
North
The staffing rations on 11 North which is a hematology unit were
decreased several years ago because so much chemotherapy was
delivered as an outpatient. However, staff began to verbalize that the
acuity was changing on the unit and in particular, the night workload was
difficult to manage. The manager and finance officer were able to
demonstrate the need and the 12hours of RN coverage was added per
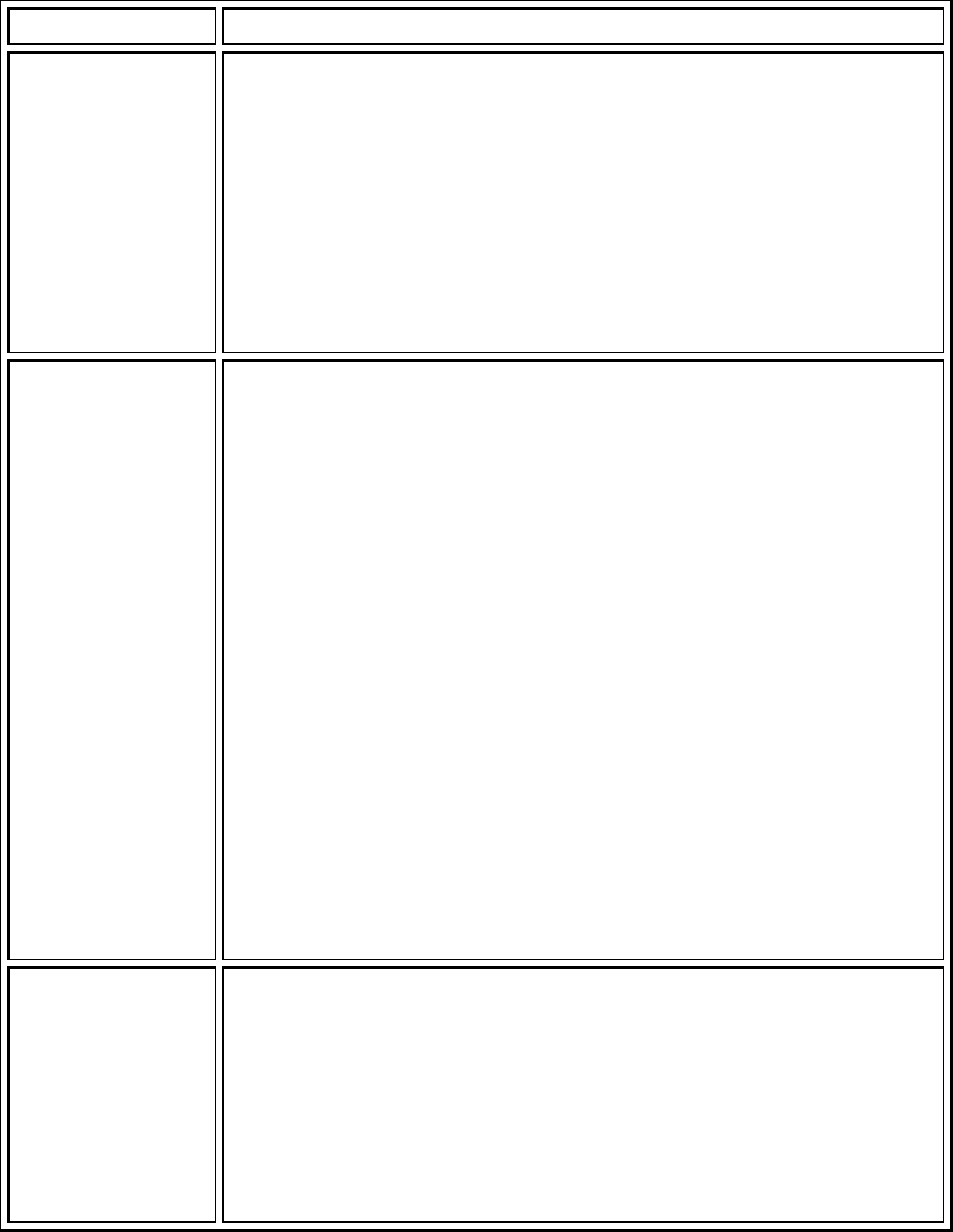
Transformational Leadership
Visibility, Accessibility and Communication (10)
109
day to the staffing template. [TL10-Exhibit
E
-1-Staff Meeting Minutes]
100 Oaks Women’s
Health Shift
Changes
Patient Care Technicians in the 100 Oaks Women’s Clinic requested 10
hour work days instead of 8 hours work days. This would allow them to
work 4 days a week instead of 5. After reviewing the request, the
manager determined that the needs of the clinic would be well served by
providing a schedule with 9 hour shifts and a ½ day on Friday. The Friday
is split with some staff working in the a.m. and some in the p.m. After a
pilot, the decision was made that the shift change was advantageous to
the work place and to staff. The change has now been fully implemented.
[TL10-Exhibit F-1-PCT 9 Hr Staffing Template]
Clinic Scheduling Stephanie Nelson, RN, Clinical Nurse Coordinator recognized patient flow
was hampered by the way patients were scheduled on Dr. Kaufman’s
template for urodynamic testing. Often these patients were new to the
practice and needed to be seen by Dr. Kaufman prior to their test being
performed. Stephanie requested that Dr. Kaufman’s template be
changed to reflect his actual practice pattern instead of 45 minutes after
actual testing occurred. There was also a need recognized for a special
procedure slot for new medication Dr. Kaufman was administering. The
procedure needed to be done in the treatment room with a sonesta
chair. This required that the team collaborate to accomplish this
complicated scheduling. Stephanie spoke with Gail Bauer and Leslie
Denton the manager of the area and they worked to have the
Macroplastique appointment placed on the schedule at 1300 to allow for
procedure to be done while the last UDS was being accomplished in
adjacent room without interference. The scheduling change also allowed
the staff to ensure all of the proper equipment for special procedure was
in place in the early am for procedure to be done @ 1300.
Development of
Standard roll-out
process in the ED
During Karin League’s, BSN, RN masters program in Health systems
management through the Vanderbilt University School of Nursing, she
had the opportunity to complete 210 practicum hours with Brent
Lemonds, RN. Brent is the Administrative Director for Emergency Services
and provided Karin with the opportunity to observe the challenges of
leadership in a large, fast paced, high risk area that experiences change
at a phenomenal pace.
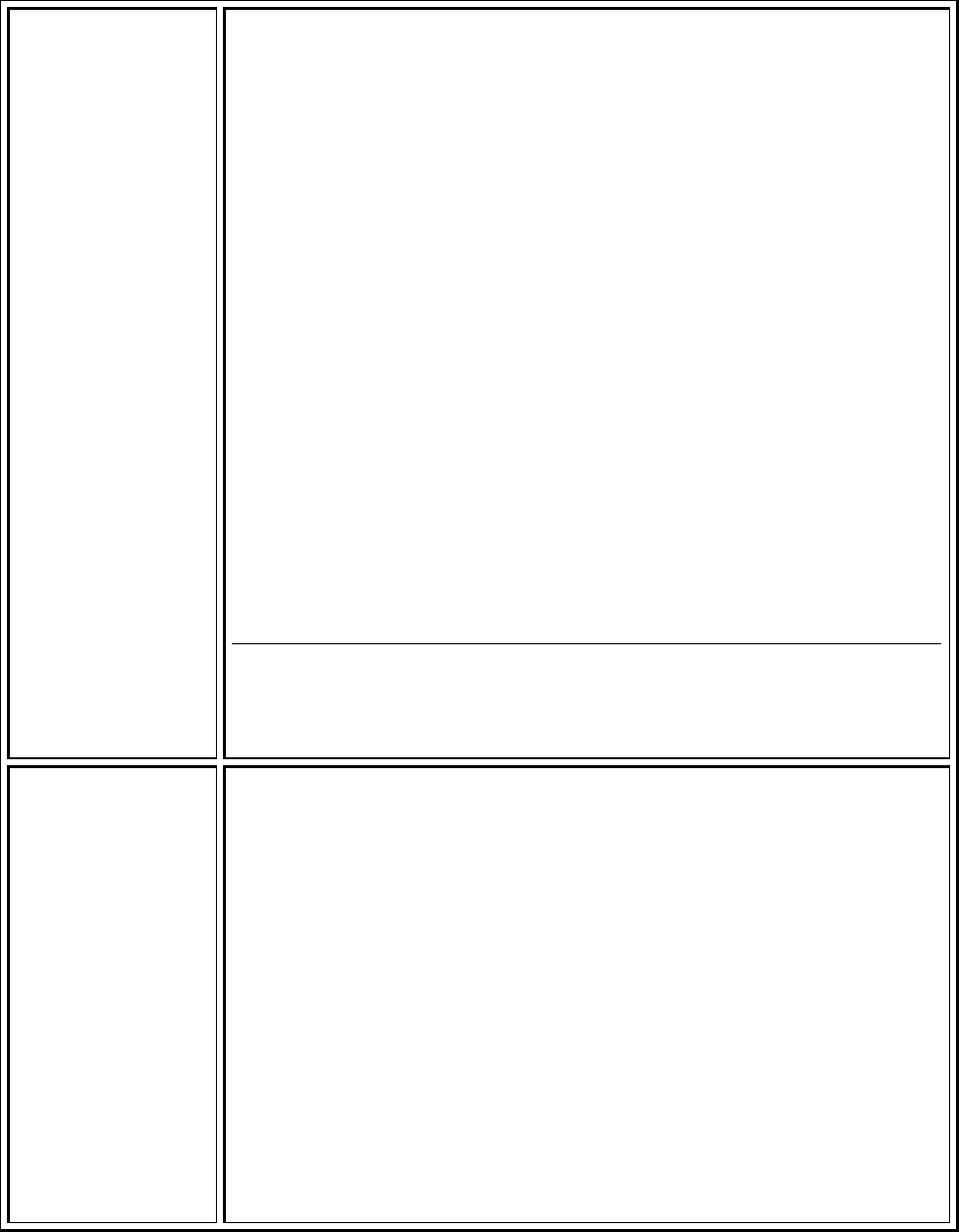
Transformational Leadership
Visibility, Accessibility and Communication (10)
110
Karin had a passion and interest in quality. She chose a practicum
project that would fit with the department’s need for change
management tools around quality, evidence-based practice, and process
improvement. Brent and Karin worked together to develop the Standard
Rollout Process tool. The tool is based on multiple theories including
Lewin’s theory of Change, Stetler Model Theory, and Roger’s Diffusion of
Innovation. Other evidence included in the development included human
factors studies and the use of tested tools such as PDSA, Gap analysis,
and SWOT analysis.
The resulting product was designed to assist teams to clearly define
their goal for change, cultivate the stakeholders involved, develop an
action plan with a timeline and clear accountability, communicate the
plan effectively, and utilize PDSA cycles for improvement and
sustainability.
Under Brent’s leadership, the Emergency Department and VCH
PACU/Holding have utilized this tool for the past year. There are several
examples of its use at
http://www.mc.vanderbilt.edu/root/vumc.php?site=adulted&doc=25041
[TL10-Exhibit G-1-Standard Rollout Presentation, TL10-Exhibit G-2-
Standard Rollout Process]
Hand washing
Foam in the PACU
In the PACU, it is difficult to have foam to wash hands with close to the
patient because there are no walls between patients, to mount hand
washing foam. If someone comes to the bedside to see the patient, there
is a distance that they must walk to get to the foam. At the request of
the nurses, Betty Sue Minton, RN, MSN placed foam on the wall behind
the patient slot, but to get to it, you had to come into the slot and reach
behind the patient to foam your hands. Therefore, the foam on the wall
behind the patient was difficult for physicians to use.
Betty Sue knew that each PACU slot had a bedside table that is usually at
the foot of the stretcher and that would be a good place for the foam to
be located. A nurse could foam their hands before they went into the
slot to see the patient and then again as you were leaving the slot. Plant
Ops built a round flat surface that attaches to the side of the bedside
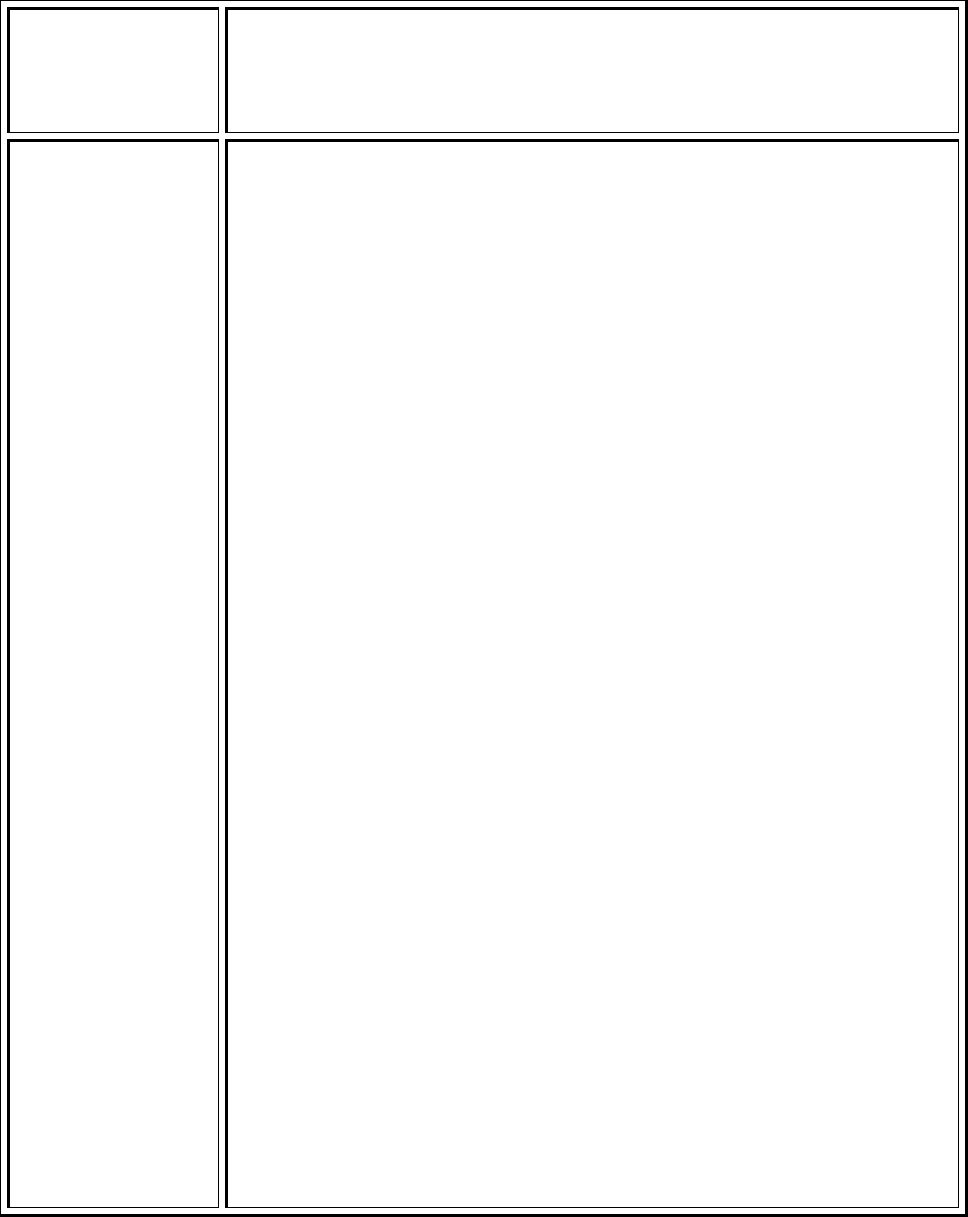
Transformational Leadership
Visibility, Accessibility and Communication (10)
111
table. The hand washing foam is mounted on the round surface. It takes
up no room on the top of the bedside table, so it is still very usable for
patients and the staff. [TL10-Exhibit H-1-PACU Hand Foam]
ECMO
Improvement
ECMO Specialist (made up of RN’s and RRT’s) work very well
collaboratively and during a PM&I (Quality Review meeting) the team
members pick patients to present. We review every patient that goes on
ECMO. The center does a large volume of ECMO patients and thus,
reviews up to 6 patients in one session. The team members are given
guidelines to present. This gives the team members the opportunity to
express their concerns and also hear what the physicians were thinking
during this process. It has led to multiple open discussions and changes
including the one below.
Daphne Hardison, RN became the manager in January 2009 and had
noted some process issues and inconsistency in the way prime blood was
“treated”/buffered. The ECMO circuit was usually primed with 2 units
PRBC’s. The blood product was buffered so when patients go on ECMO
and are exposed to the blood it not only is anticoagulated but has
electrolytes and gasses in a range to prevent the heart from going into a
stun picture. The team had different ideas on how to make this the
correct gas and what is acceptable. Because the protocols requested a
physician order, Daphne required all team members to go to the
physician and get an order instead of just adding different medications.
ECMO is not utilized by all physicians every day; therefore there was
even more inconsistency with the physician orders than when the
specialist did their own thing. Many team members felt it very difficult to
get the orders during the intense time of ECMO Cannulation and
requested a solution of some sort to include a protocol. Daphne took
this back to the group and facilitated a discussion where a decisions was
made to create a protocol that came from our director’s (surgical and
medical) that allowed the team members to treat the circuit gas
appropriately and independently. This has not only led to the ECMO
Specialist independence but the physicians are not expected to come up
with answers during a code situation. [TL10-Exhibit I-1-ECMO WIZ Order
Guidelines, TL10-Exhibit I-2-Minutes Medical Director, TL10-Exhibit I-3-
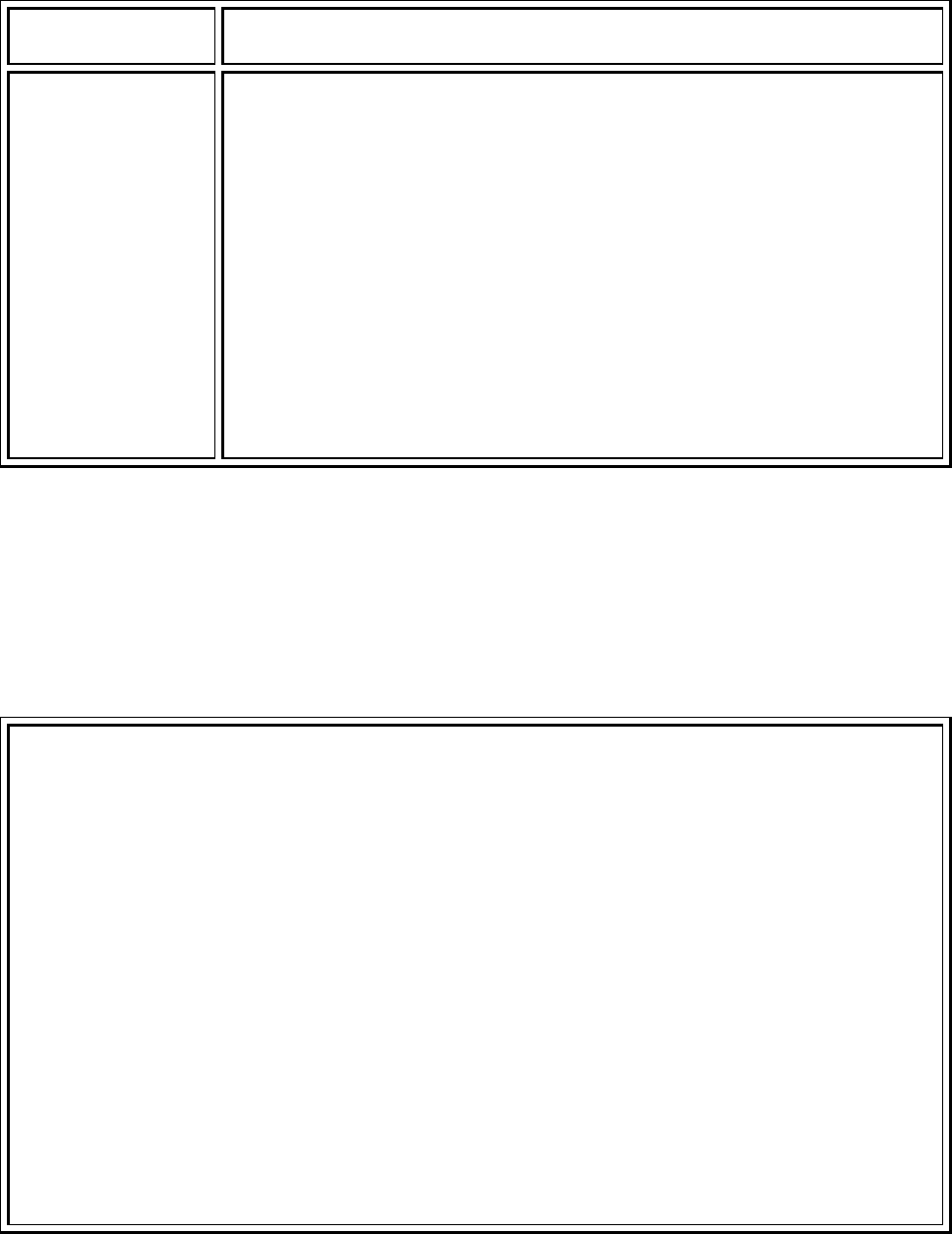
Transformational Leadership
Visibility, Accessibility and Communication (10)
112
Team Meeting Minutes Aug 2010
]
9 North and pill
splitters
When Richard Corcoran, RN, MSN manger of 9 North first came to 9
North two years ago the first step he did was round on all employees to
get to know them and identify any areas they felt needing improving
rapidly. Two items came up repeatedly – pill splitters, and pill crushers.
Nurses stated that they never were available and hunting them was a big
time waster. Within 2 weeks Richard had a pill splitter and a pill crusher
attached to each Work Station on Wheels. The pill splitters have
remained and are replaced as needed. On 9 North pill crushers moved
to the top of each unit supply care for infection control reasons this past
January. These replaced the smaller individual crushers in use prior to
that time. [TL10-Exhibit J-1-Unit Board Minutes]
“In her Own Words” – Story by Anisha Fuller, Manager 4 East, OB/GYN
“In April of this year, one of the night shift nurses, Amy Suddeath, sent me an email
stating that she had taken the initiative to investigate some cost saving measures that could be
taken in our department. I have attached her initial email, for your review.”
EMAIL FROM AMY SUDDEATH
–
APRIL 27, 2010
“Anisha,
For the past 3 years, I have complained about what a dumping ground our nurse servers are.
I know that they are intended to be helpful to staff but they are so randomly stocked that I think
we spend more time going from server to server hoping to find something than we would spend
just going to the main cell. I get so frustrated with them that it has become by personal mission
to clean them out approximately every 6 weeks or so. After cleaning them out several times, I
decided it would be really interesting to see just how much the items being stuffed in the servers
(and rarely used because no one knew they were there) were actually costing our unit in
restocking charges. I cleaned out the servers and returned everything to the main cell. Six
weeks later I cleaned them out again. I wrote down everything I returned to the cell and
contacted Karen Sterbutzel, Supply Chain Director. She provided me with a price list for every
item stocked on our cell. I used the list I had prepared from my "six week cleanup" and
computed the cost of all the items I had returned to stock just that one time. The total cost of
those items was $110.00. If every six weeks that same amount was returned to the cell, the
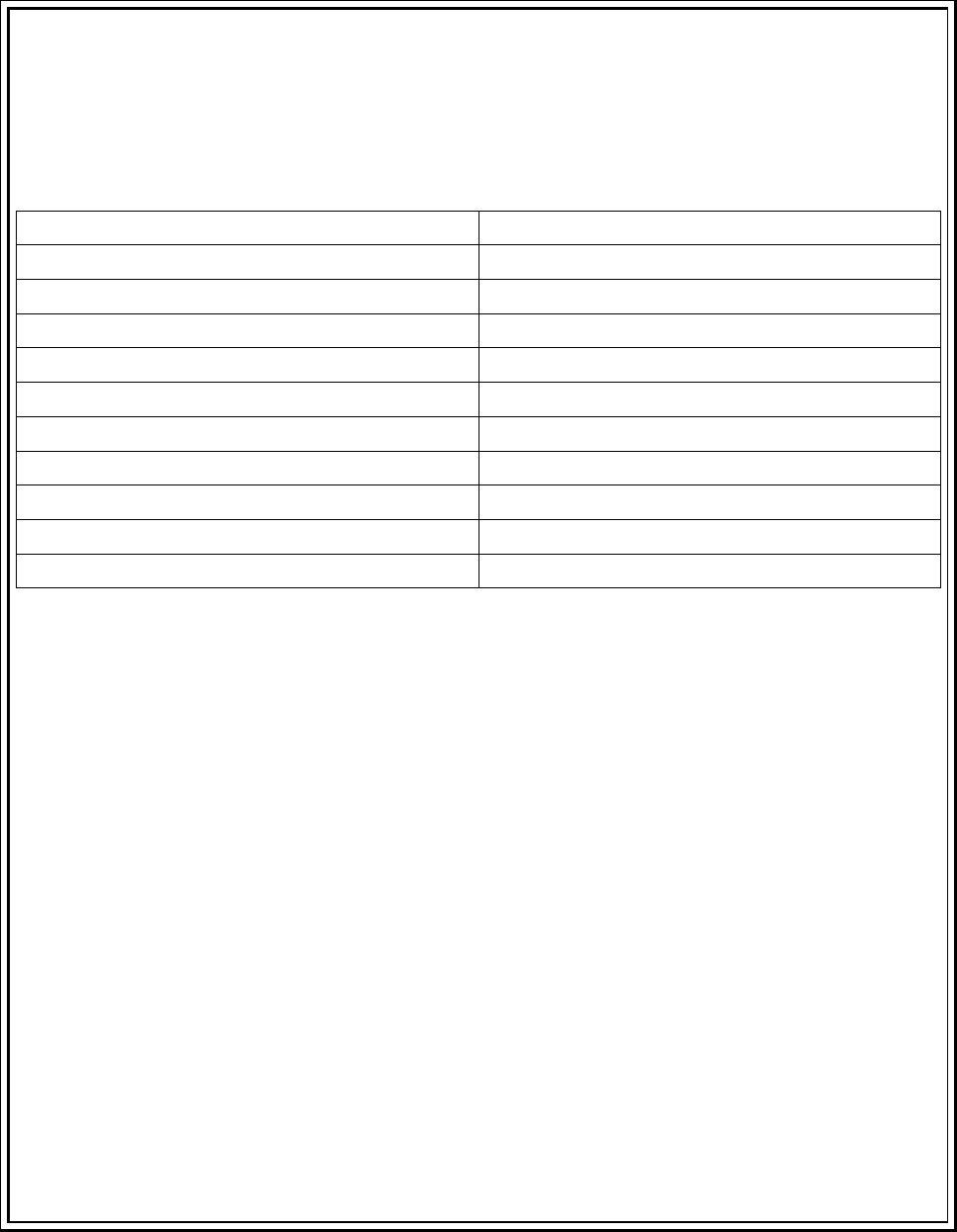
Transformational Leadership
Visibility, Accessibility and Communication (10)
113
annual cos
t
would be $952.00. I don't think a lot of our staff realize that every time they stick
something in the nurse servers, that missing item has to be restocked on the cell to maintain
par. Our patients are not paying for us to maintain par, the unit pays. Therefore, if everyone
would return items to the cell when they aren't used, the unit could save approximately
$1000.00 per year.
Here is a list with prices for some of the most frequently "dumped" items:
Specipan $0.38/ea
Pitchers $0.29/ea
Socks $0.66/ea
Bath wipes $1.42/ea
Catheter kits $ 1.88/ea
BP cuffs $2.94/ea
Bedpan $0.63/ea
Soap $0.22/ea
Shampoo $0.22/ea
Toothpaste $0.22/ea
Bath basin $0.39
I realize that we do sometimes use these things if we are lucky enough to find them when we
need them, but how often do we just go to the cell instead of wasting time looking in the
servers?
Just this past weekend, I was looking for Tucks pads in the servers and found probably 10
bags of items that looked like they were gathered in preparation to set up empty rooms. That is
a great way to be prepared especially when things are as busy as they have been lately.
However, in almost every bag I noticed that there was shampoo, toothpaste, a toothbrush,
tissue, deodorant, blue or brown socks, and a package of bath wipes. Most of our patients don't
need any of those things because they usually bring all of those things with them. If you add up
the cost of all of those items it is $4.08 per patient. If you estimate that we admit 8 patients per
day, that same setup would cost our unit $32.64/day or $11,913.60/yr! That's almost
$12,000.00 a year the unit could save just by giving those items out on a request only basis. I
have worked at other facilities where a "room setup package" was charged to the patient on
admission and extra items were also charged when requested. I don't see Vanderbilt ever doing
that but we could definitely be more conservative with those items instead of including them
with every room setup.
Transformational Leadership
Visibility, Accessibility and Communication (10)
114
One last thing, during one of my server cleanouts I found 25 BP cuffs. Some were still
wrapped and were returnable to the cell. Most were unwrapped and there was no way to tell if
they were used, from an isolation patient's room, or were defective and just stuffed in the server
for convenience. I ended up throwing away all of the unwrapped ones for patient safety. BP
cuffs are $1.94/ea and were the most frequently dumped item. If staff could discard them when
they are worn out and only remove them from the cell when they are replacing old ones, lots of
money could be saved.
My point in this project is to make all staff aware that it is really important to return things to
the cell if they aren't going to use them. The unit is charged for every item that sits in the
servers unused. I know we all get busy and sometimes don't have time to do the most cost
effective thing. Would a box, placed at each nurses station to put unused items in, be helpful?
Maybe our volunteers could help us with restocking those items? Any other suggestions?
I think that we all do our best in using our resources wisely, but sometimes need a little
motivation to improve. I hope everyone finds this information informative and helpful. I have a
price list of every item on our cell, so if anyone is curious about how much something cost I
would be happy to let you know.”
Thanks!
Amy Suddeath, RN
“In summary, she had noticed that many of the non-chargeable supplies were being
haphazardly stored in the cabinets (nurse servers) throughout the unit. This practice was
causing costly clutter, and resulted in inaccurate par levels in the unit storage room.
Amy made the suggestion that we create specific storage locations among the existing servers,
and formally organize what is placed in them. I thought it was a great idea, and supported her
taking it to our Unit Board meeting. She was put on the agenda, and presented her findings to
the department. Everyone was in agreement that we could better organize how we store
supplies, and they voted to adopt Amy’s suggestion.
Together, the staff decided which cabinets would be best suited for centralizing linens
and supplies. Five cabinets were designated for this purpose. Labels were made, and the
cabinets were organized to one standard. Since then, the staff have maintained how the
servers are utilized. Amy still does her six-week “round-up,” but she finds less and less clutter
each time.

Transformational Leadership
Visibility, Accessibility and Communication (10)
115
I have helped support her project by encouraging her to present to Unit Board, and
endorsing her project in that forum. Empowering her to take action on something she identified
as a problem has added to an atmosphere of staff empowerment and recognition for innovative
ideas. I facilitated the coordination of support needed to initiate the organization of her project,
and have continued to do so. Amy has drafted several emails to the staff, and asked that I send
them out on her behalf. This shows that I support her efforts, and request that others do, as
well.
It has not been a long-standing project, but it will be interesting to see if our non-
chargeable costs to the unit decrease over time. I applaud Amy’s drive and persistence, and am
proud to be her manager. She’s a great member of the team. Incidentally, Amy received her
RN3 while working on this project.”
“In Her Own Words”
Submitted by Christine Kennedy, MSN, RN, Administrative Director, Adult Medicine –
September 7, 2010
“At Vanderbilt University Medical Center, an interdisciplinary team, the Pain
Management Task Force, has been working on improving pain management assessment and
reassessment with a particular focus on streamlining documentation in our charting system
Horizon Expert Documentation (HED). One specific objective was to provide direction to the staff
to choose and use one pain scale appropriate to the patient. After our Pain Management
Guidelines were updated in November, 2009, the Pain Management task force had been
working with staff to get their input as to how we could improve our documentation format
related to assessment and reassessment of pain.
During focus groups with staff, it was identified that not all staff understood which pain
scales should be used for patients who were “able to self report” versus those patients who
were “unable to self-report”. For example, some staff members were using the Wong-Baker
Faces scale for patients who were “unable to self report”. By definition, the Wong-Baker Faces
scale is to be used for a patient who is able to self report. This scale is typically used by a child or
someone who prefers to point to a face rather than using the numeric rating scale (NRS). One
change made in a release that took place on July 19, 2010 was to differentiate the scales for
patients “able to self report” from those patients who are “unable to self report”. Patients who
are “unable to self report” are typically non-verbal patients who cannot communicate their

Transformational Leadership
Visibility, Accessibility and Communication (10)
116
needs. In order to identify if patients are in pain, staff observe physiological or behavioral cues
to determine if the patient is in pain. The following scales: FLAAC, NIPS, NPASS, and PAIN AD,
are summative scales used at Vanderbilt for patients who are “unable to self report”. There are
some patients for whom we cannot use any of these summative scales and for these patients
the nurses describe physiological or behavioral cues to try to determine if patients are in pain.
After the July 19 release of changes in HED, our system support staff and educators
rounded on staff to help explain the rationale for these changes. In general this change was well
accepted and during rounding with staff this was generally seen as improvement.
There was one concern identified. It was identified by users/staff that due to the change
in format, there was no longer an option listed under the pain assessment drop down boxes for
patients who cannot self-report pain. This was identified by staff, communicated through the
HED Advisory committee and forwarded to the Pain Management Task force. A solution was
identified by the Pain Management Task Force and vetted with staff. The solution was to add
two descriptors, one each under behavioral cues and physiological cues. The purpose of adding
these options was to allow the nurse an indicator for behavioral and physiologic cues that
suggests the patient is not in pain. This can be used for the shift assessment as well as for
reassessment after interventions.
Deborah Ariosto, MSN, RN, Director of Patient Care Informatics was instrumental in
helping to facilitate conversations and devise the redesign released on July 19, as well as the
additional simple solution. With the help of Nancy Rudge with HED, the additional changes
requested by the staff were released to the organization on August 31, 2010. We appreciated
the feedback from our clinical staff and appreciated the quick response from informatics and
system support staff for implementing this small but important change. At this time, the
feedback from this change is that it has addressed the concern identified by the staff.”
[TL10-Exhibit K-1-Pain TF Meeting Minutes, TL10-Exhibit K-2-Pain Management HED Screen
Update, TL10-Exhibit K-3-Pain Documentation Revision]
Transformational Leadership
Visibility, Accessibility and Communication (10 EO)
117
Visibility, Accessibility, and Communication
Source of Evidence 10 EO
Describe and demonstrate changes in the work environment based on input from the direct-
care nurses.
Transition from Systems Support Specialist to Clinical Application Specialist
Purpose/ Background
The use of informatics systems has become extremely important for nurses to
accomplish patient care. Vanderbilt develops many of the informatics tools nurses use and the
pace of change is great. For many years, the System Support Department of Informatics which
supports end users in the clinical areas has reported to the Executive Chief Nursing Officer. The
role of the “Systems Support Specialists” (SSS) on that team has largely focused on
implementation of new systems. After implementing two large-scale, complex clinical nursing
applications back to back, our institution realized there was a problem. User feedback from
nurses indicated the Systems Support Department is great at implementation of systems, but
not as accessible as they would like for ongoing support. A goal was established by the team to
allow Systems Support to respond in real-time to increasing regulatory requirements without
additional FTE’s and to increase user independence and proficiency in all clinical computer
systems. The hypothesis was that user-based versus centralized support will increase overall
institutional satisfaction with systems support services. This plan that responded to needs of
nurses began the transition of Systems Support Specialist to Clinical Application Specialist.
The project was based on the following information.
• User feedback was that Systems Support provided great support for implementation of
systems but there was dissatisfaction with accessibility for ongoing support.
• Ever increasing regulatory requirements and scrutiny by regulatory bodies required
users to be able to meet documentation requirements and use systems to leverage their
understanding of the patient status and patient needs. Users must be knowledgeable of
the most effective use of tools and processes, and there needed to be iterative
enhancement to those tools and processes for documentation
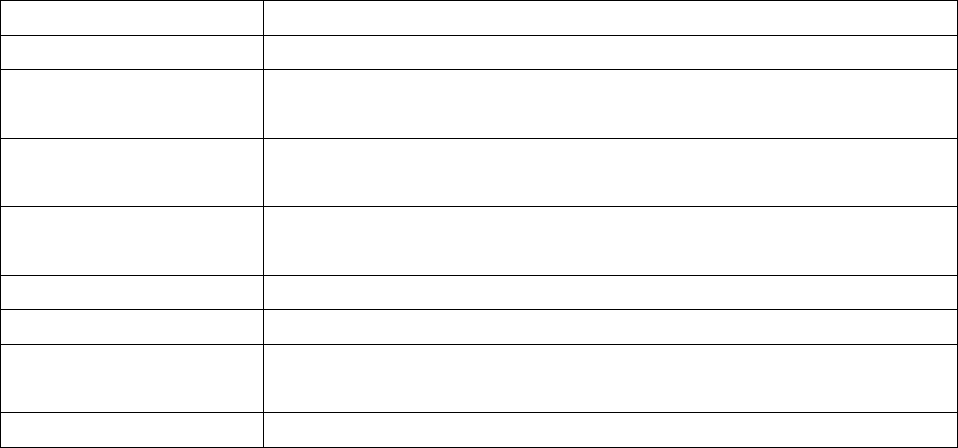
Transformational Leadership
Visibility, Accessibility and Communication (10 EO)
118
• The increasing size and complexity of the organization created a need for new support
strategies.
• SSS staff needed an opportunity to expand their skills and leadership abilities.
• Customers should become less reliant on SSS and be able to use all informatics systems
more effectively and independently.
• SSS must demonstrate the success of informatics system from a user’s perspective as
well as a systems perspective.
Table TL 10 EO – 1: Participants
Karen Hughart, RN, MSN Director of Systems Support Services
Gwen Holder, RN, MSN Assistant Director of Systems Support Services
Sara Seaman, RN, BSN Clinical Applications Specialist for Adult Neurology/Epilepsy & Neuro
ICU
Lillian McGehee, RN,
MSN
CAPS for Adult Surgical ICU, Surgical Step-down, & General Surgery
unit
Ron Reed, RN, ADN CAPS representative for VCH covering general surgery floors for
young/adolescent as well as medical infant to adolescent
Tom Mack, RN, BSN CAPS Representative for adult medicine floors and Medical ICU
Lisa Grunwald RN, ADN CAPS Neonatal Intensive Care Unit
Valerie Kibler, RN, NP CAPS representative for adult colorectal, urology, orthopedic, and
general surgery units
Sara Winters RN, BSN Clinical Application Support Team Lead
Approach/Methods
The first step in developing a plan for area based Systems Support Specialists was unit
selection. CAPS would be assigned to a unit or group of units that complement one another.
Variables influencing the development of CAPS assignments to units or “pods” included the
following:
“sister” units (same management) would be grouped together
patient flow from ICU to step down/general care floor should be considered in the
groupings
Transformational Leadership
Visibility, Accessibility and Communication (10 EO)
119
acuity, number of staff, number of patients, geography should be considered
Once assignments were made, the teams began to move toward implementation.
Clinical Application Specialists (formerly Systems Support Specialists) met with unit leadership
to establish relationships, expectations, desired outcomes, and boundaries. They introduced
the idea of Clinical Application Specialists to staff nurses and used that time for information
sharing and to begin to build relationships with nursing staff.
The next phase was an observation phase. During this time, CAPS observed workflow in
their assigned areas and were oriented to the unit practices. They gathered information via a
survey focusing on current use and knowledge of clinical applications. This information was
used to prioritize education efforts.
The survey yielded information on:
Nursing documentation systems including medication bar-coding
Application downtime procedures
Electronic Medical Record
Provider order entry system
[TL10 EO- Exhibit A-1-Computer Applications Support Survey]
The next phase of implementation was the identification of priorities and ongoing
support. The CAPS assessed educational and work process simplification needs of the staff to:
Identify opportunities to leverage existing tools to help meet clinical and
operational objectives.
Identify potential systems enhancements that would make the tools more
effective/efficient
Prioritize needs and develop a plan to address priority needs
Implement the plan
Evaluate and revise objectives and strategies on an ongoing basis
Provide support on the units
Transformational Leadership
Visibility, Accessibility and Communication (10 EO)
120
Answer questions about computer applications during daytime hours
Explain computer related processes
Troubleshoot computer problems as they happen
Follow up on issues that arise
Decrease the time between questions and answers
Engage in problem solving alongside staff and follow through to resolution
It was recognized that there was a need for on- going learning for the CAPS. Learning
needs were met through collaboration across CAPS in CAPS meetings that were held every two
weeks. This provided an opportunity to share information and trends they had observed on
CAPS units. The meetings provided a forum for preliminary review of tools developed in
response to education requests, suggestions, and issues experienced by nursing staff with
clinical applications. CAPS met with unit leadership and unit boards to discuss ongoing work
and priorities or obtain feedback. [TL10EO-Exhibit A-2-CAPS Overview]
Outcomes
A goal of the project was to have CAPS staff on the unit 80-90% of the time of their
worked hours in order to be available to staff when the questions arise.
From November 15 – December 15, 2009 CAPS spent 481 man hours on the units. There
were a total of 6 CAPS representatives covering 18 units/pods. These 6 CAPS employees worked
a mixture of 30 – 40 hours per week.
The initial goal was that CAPS would spend 80-90% of work time on the units.
Initial Outcome – CAPS time spent on units:
• Average for all areas = 68%
• VCH = 66%
• VUH = 63%
• Round wing = 75%
Based on the initial results the goal was modified to 60-70% of work time spent on units. This
was found to meets the needs of the users on the units as well as SSS central office work
Transformational Leadership
Visibility, Accessibility and Communication (10 EO)
121
The areas where the CAPS provided assistance included:
• Hardware Issues
• Implementation Support
• Staff Orientation
• Management Team Efficiency
• Troubleshooting
• Problem Resolution
• Project Preparation
• Quality Improvement
Examples of improvements made based on presence of the CAPS are described here.
Hardware
• On the 8
th
floor of Children's Hospital a need was recognized Workstations on
Wheels (WOWs) were in demand for multiple groups. Reorganizing existing WOWs
to place scanners on machines used by nurses who give meds improved overall
satisfaction, maintained hardware for all groups and did not affect unit budget.
• On the round wing units more wireless scanners were needed to replace tethered
scanners when large numbers of isolation patients were on the unit. Following
intensive care unit moves to the critical care tower (with all new equipment) our
CAPS person was able to negotiate two “new” wireless scanners from the “old” ICU
space at no cost.
Implementations
• Children's hospital reported “quick and painless rollout of Falls Risk and Braden Q
Indicators”
• Tamper resistant printers and pharmacy upgrades were supported
• Large scale efforts to streamline the three ICU moves to critical care tower, including
testing of all hardware functionality, printing capability, and behind the scenes
changes for location compatibility primarily conducted by the 3 ICU CAPS
representatives
Transformational Leadership
Visibility, Accessibility and Communication (10 EO)
122
• Plan of care rollout for the 8th floor of Children’s hospital in two weeks time
educating over 100 staff in coordination with the educator
Staff Education and Orientation
• 20 or more new staff in Children's hospital received on-on-one review of technology
tools available to them, followed by requests from seasoned staff to also participate
in learning experience
• Mini lunch education sessions on 9 south for discussion of downtime process
improvement
• Training on unit specific applications such as pre-orders and plan of care at time of
need.
• Encouraging StarPanel use in NICU by customizing views for staff and illustrating
features available to them
• Assisted physicians on MICU to gather information and links to allow viewing of
IMPAX images from home
Management Team Efficiency
• Detailed assistance to leadership team for retrieving and searching for quality
safety measures on patient records, including those that are discharged, and
chart audit reviews
• Charge nurses on MICU were taught how to most proficiently access “fix it now”
reports
• 9 north charge nurses had white board indicators customized to assist in
managing quality care goals
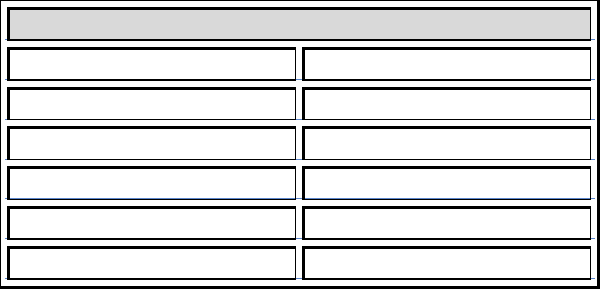
Transformational Leadership
Visibility, Accessibility and Communication (10 EO)
123
Trouble Shooting/Problem Solving
• Directly taking calls during daytime hours to reduce wait time on calls to the help
desk – following up with help desk to manage data collection and trends of issues
• From routine CAPS rounding learned that SICU had certain lab screens they are
accustomed to seeing that were not displaying correctly after the move to the
Critical Care Tower. Through detailed follow u p discovered that certain screens in
HEO were “hard coded” to the 3N/C location only. Resulted in thorough evaluation
and reconfiguration of three similar instances.
Project Preparation and Quality Improvement
• Anticipating needs of NICU leadership and staff for implementation of Admin-Rx
during 2010
• Improvement of Admin-Rx scan rates following embedded CAPs representative on
Round Wing (Table 1 below)
Empowering nurses with suggestions for HED improvements to take ideas to HED advisory
committee. Several have been approved!
Table TL 10 EO – 2: Admin RX Scan Rate Trend
Admin RX Scan Rate Trend
Month S34 total
February 73%
March 84%
April 96%
May 97%
June 99%
Next Steps
• Expanding CAPS role to more areas in the medical center
Transformational Leadership
Visibility, Accessibility and Communication (10 EO)
124
• Continuing to manage expectations with controlled growth of the program
• Ongoing efforts to maintain quality initiatives housewide with direct impact support
• Submitted abstract to ANIA 10/08 - Sara Winters RN BSN and Valerie Kibler RN NP
[TL10EO-Exhibit A-3-CAPS Outcomes]
CVICU Ultrasound Guided Peripheral IV Insertion
Purpose and background
The CVICU staff, leadership and medical directors were interested in reducing the rate
and the risk of central line infections. This work was initiated by Kirk Krokosky, RN who was a
night shift staff member in the CVICU at the time. They observed that some patients received
central lines because peripheral access was not possible. They hypothesized that if they could
eliminate or delay the need for central line catheters they would reduce the central line
infection rate. On a parallel course, they wanted to improve the quality of peripheral
intravenous access and patient comfort while obtaining said access.
The two primary reasons to pursue this project were:
to reduce the number of central line associated blood stream infections (CLABSI) by
decreasing the need for or delay the placement of central lines most commonly PICC
lines.
To improve success of peripheral IV insertion in patients that were considered “difficult
sticks” related to obesity, edema, known poor quality veins.
Methods/Approach
An intensive analysis was done on BSI cases that occurred during a five month period
(July-November 2008, n=7 cases).
It was found that medical cardiology patients who acquired BSI were all related to the
presence of a peripherally inserted central catheter (PICC).
Based on this analysis, in early 2009, all staff were re-educated on care and
maintenance of central venous catheters, including PICC lines.
Transformational Leadership
Visibility, Accessibility and Communication (10 EO)
125
As a parallel course, a process to find an alternative to inserting PICC lines in patients
previously identified as non-peripheral intravenous (IV) access candidates was pursued.
These candidates were determined by the presence of:
o Edema
o Obesity
o Unsuitable or poor quality veins
o History of multiple attempts
o A review of literature revealed that ultrasound guided venous access technique
has been used with success by physicians in the emergency department setting.
A competency based protocol for nursing insertion of ultrasound guided peripheral IV
access was developed.
The data demonstrated a significant reduction in PICC usage (Figure 2) and a subsequent
decrease in BSI rates.
[TL10EO-Exhibit B-1-Ultrasound Guided IV Insertion Policy, TL10EO-Exhibit B-2-Ultrasound
Guided IV Manual, TL10EO-Exhibit B-3-QCOR Ultrasound Poster-ONSITE]
Table TL 10 EO – 3: Participants
Kirk Krokosky BS, RN,CCRN Developed project, conducted in-services
Jeannie Bryd, MSN,RN Project oversight
Kathleen Burns Med, RN Assisted with development & provided guidance on in-services
and data collection.
Lee Parmley, MD project oversight, collaboration at the provider level with the
Vascular Access Group
John McPherson, MD project oversight, collaboration at the provider level with the
Vascular Access Group
Chad Wagner, MD project oversight, collaboration at the provider level with the
Vascular Access Group
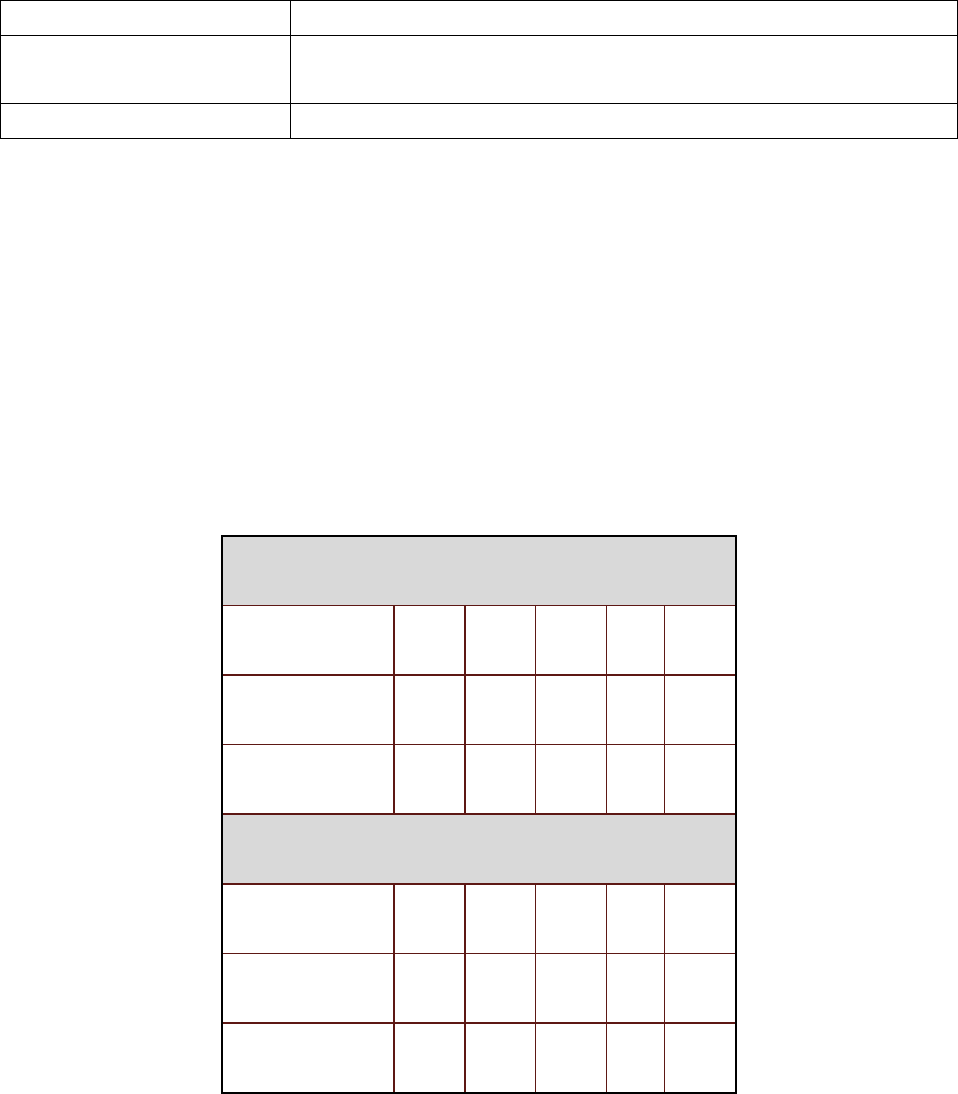
Transformational Leadership
Visibility, Accessibility and Communication (10 EO)
126
The CVICU Collaborative
Committee
provided data review, support and endorsement of the project
Staff nurses of the CVICU
Outcomes
The table below compares success rates of lines placed traditionally (no ultrasound) vs.
those placed with ultrasound guidance. Most noteworthy is the success rate on first attempt of
64% [with ultrasound] up from 27% (without ultrasound). As for PICC insertions the top graph
in figure 2 shows a dramatic decrease in PICC insertions in the first four months of the live
project (Jan- April 2010). Graph 3 shows an encouraging trend downward in the number of
blood stream infections.
Table TL 10 EO – 4: Success Rate with ultrasound vs. no ultrasound
Traditional Peripheral IV Technique
Attempts 1 2 3 4 5
# of Patients 6 6 6 0 4
Success rate 27% 27% 27% 0% 18%
Ultrasound Guided Insertion Technique
Attempts 1 2 3 >3
# of Patients 21 9 3 0
Success rate 64% 27% 10%
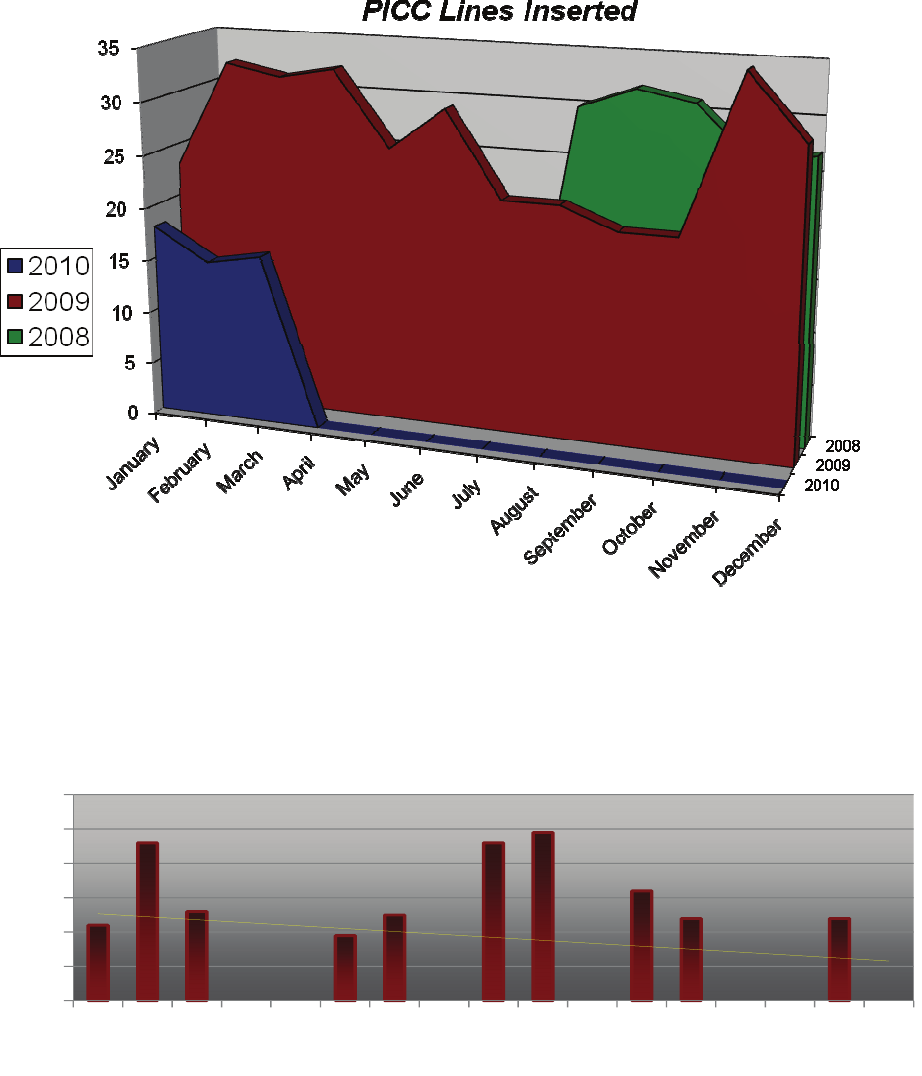
Transformational Leadership
Visibility, Accessibility and Communication (10 EO)
127
Graph TL 10 EO – 1: Decrease in PICC Lines Inserted
Graph TL 10 EO – 2: Blood Stream Infection Rates
0
1
2
3
4
5
6
Nov Jan 09 Mar May July Sep Nov Jan 10 Mar
Blood Stream Infection (BSI) Rates
Transformational Leadership
Visibility, Accessibility and Communication (10 EO)
128
Summary
The CVICU has seen a significant reduction in PICC line usage and subsequent reduction
in CLABSI rates as a result of the implementation of ultrasound guided peripheral IV insertion.
The project has been a success and the area is moving forward to train more staff in the
technique. To date there have been no major complications related to the technique. The
CVICU staffs have been asked to place lines in other units and currently the Burn Unit is
developing its own program based on our materials and data. The use of ultrasound guided
technology by specially trained nurses has increased the success rate of obtaining peripheral IV
access. As a result, the reduced need for or at least delayed placement of central access was
achieved. This reduction has brought about a downward trend in BSI rates.
